14.1 Introduction
A child or young person with learning difficulty or disability may
require special educational provision. The definition of a child or
young person with special educational needs or disabilities (SEND) is
set out in the Children and Families Act 2014 . Local authorities
have statutory duties and responsibilities for this group of children
and young people. These are outlined in the Children and Families Act ,
supporting guidance, and the SEND Code of Practice . These include
information regarding how they are categorised and supported through
education, health and care plans (EHCPs) and SEND support.
SEND can affect a child or young person’s ability to learn
through:
- behaviour or ability to socialise and make friends
- reading and writing
- ability to understand information and concepts
- concentration levels
- physical ability.
Wandsworth considers children and young people with SEND, and the
quality of support they receive, to be a significant priority at a local
authority level. Nationally, the number of pupils classified as having
SEND has increased for a fourth consecutive year. Wandsworth has a
higher-than-average number of pupils recorded as having SEND within the
school population compared with statistical neighbours and nationally.
It also has a higher-than-average proportion of EHCPs within the
resident population.
There are a number of predictive factors for the development of young
people who have SEND. Many may be a result of biological factors but
there are a number of social factors which may make a child more likely
to develop a special need or disability. Factors explored include birth
and maternal indices, age, gender and ethnicity, socio-economic
disadvantage, being a looked after child, and crime.
There are some limitations to the data quality and information within
the Special Needs Assessment Service. Variation across datasets with
regards to population and categorisation of need, and the complexity of
needs, means children may be subject to multiple services who store
information across different, often incompatible, systems. The concept
of unmet need has been explored in certain cohorts within the SEND
population where there are potential gaps, and it is important the local
area considers ways in which these can be resolved.
Research has been undertaken to gain some insight into interventions
and approaches that work according to the evidence base, whether this be
through guidance or looking at what is being done in other local areas.
This may help inform future service provision, improve support and
services currently offered, and specifically target areas of unmet
need.
14.2 Needs of Children and Young People with SEND
The level of need within the Wandsworth population is explored,
highlighting significant increases in the number with EHCPs over the
previous years, and higher than average proportions of EHCPs and SEND
support within the school population. Cross border movement is one
possible reason for this due to large numbers of out of borough
residents accessing educational provision within Wandsworth,
particularly specialist provision.
Various specific areas of need are explored in more detail and key
findings indicate:
- a significant and increasing prevalence of autism spectrum disorder
(ASD) as a primary need
- high prevalence of social, emotional and mental health needs in
Wandsworth in comparison to the national picture, and a concerning
incidence among Black Caribbean pupils, highlighting an ongoing issue
with overrepresentation in certain ethnic groups
- high level of speech, language and communication needs (SLCN) which
need to be carefully considered among the English as an additional
language (EAL) cohort
- good educational outcomes for SEND Support, but not so good for
EHCPs with issues regarding EHCP timeliness
- Issues in the transition process from children’s to adults services,
meaning planning is not always happening early enough to the detriment
of the young person’s health.
Children and Families Act 2014
The Children and Families Act (2014) (Part 3) states that a child
or young person has SEND if he or she has a learning difficulty or
disability which calls for special educational provision. As defined in
this 2014 Act, a child of statutory school age or a young person has a
learning difficulty or disability and significantly greater difficulty
in learning than the majority of others of the same age or has a
disability which prevents or hinders making use of facilities generally
provided for others of the same age in mainstream schools or mainstream
post-16 institutions. Children of statutory school age has a learning
difficulty or disability if he or she is likely to fall within the above
definition when of compulsory school age or would do so if special
educational provision was not made for them. Compulsory school age ends
on the last Friday of June in the academic year in which they become 16
years old. Until they are 18 years old, they must stay in full-time
education, start an apprenticeship or traineeship, or spend 20+ hours a
week working or volunteering while in part-time education or training .
Under Part 3 of the Children and Families Act 2014 a local authority
in England has a duty to exercise its functions to identify all children
and young people in the area who have or may have SEND. Local
authorities and partner commissioning bodies are also required to put in
place joint commissioning arrangements to plan and jointly commission
education, health and care provision for children and young people with
SEND.
Major reforms to the support system were implemented by the
government as part of the Children and Families Act 2014. The changes
were intended “to put children and parents at the heart of the system”.
Some of the key aims were to ensure children’s needs would be identified
earlier, families would have more say in decisions, and support services
would be better integrated. The Act also replaced Statements of Special
Educational Needs and Learning Difficulty Assessments with the
Education, Health and Care Plan (EHCP). It covers support for pupils
with special educational needs and disabilities (SEND) from birth to 25
years of age . Since 1st September 2014, all new
statutory assessments have been made under this new system.
Under the Act, support for children with SEN is categorised under the
following:
- SEND Support – the majority of children and young people with SEND
will have their needs met through the graduated approaches embedded in
early years settings, schools and colleges
- Education, Health and Care Plans (EHCPs) for children and young
people up to the age of 25 years who require more support than is
available at SEND Support. These plans identify the educational, health
and social needs, identify the outcomes to be achieved and define the
additional support needed to enable the child/young person to achieve
the outcomes.
In order to make sure the key messages in this JSNA are clear,
information largely correlates with the two abovementioned cohorts:
those on SEND Support (data includes children and young people attending
Wandsworth schools, whether they are resident in the Borough or not),
and those with an EHCP (data refers to children and young people
resident in Wandsworth, whether they attend school in or out of Borough
i.e., resident population). However, we have occasionally used a third
cohort of those within the school population with EHCPs to give a fuller
picture of the school population with SEND in relation to their peers
without SEND. In January 2020, 75% of the SEND (Reception to Year 11
pupils) were also in the school census.
As part of the reforms, in 2014, the Department for Education and the
then Department of Health jointly published the SEND Code of Practice
(2015), providing statutory guidance on duties, policies and procedures
relating to Part 3 of the Children and Families Act 2014 and associated
regulations. Local authorities must have regard to this guidance .
Local authorities have a crucial role to play as they have statutory
responsibility for ensuring that children, young people and families
receive the necessary support. The SEND Code of Practice highlights the
need for local education, health and social care services to work
together to provide the right support for pupils with SEND to ensure
they can achieve the best possible outcomes.
Pupils with SEND
Currently children and young people with SEND are a national priority
and challenge, with the number of pupils with SEND having increased for
the fourth consecutive year, following a period of year-on-year
decreases from 2010–2016. According to the Department for Education
(DfE) , over 1.3 million pupils in England were
recorded as having special educational needs and disabilities (SEND) in
January 2020, representing 15.5% of all pupils. This increase has been
driven by both the number of pupils with an EHCP and with SEND
Support.
Pupils with special educational needs and disabilities are some of
the most vulnerable in the school system. The quality of the support
they receive can significantly impact their life experiences,
well-being, educational attainment, likelihood of employment, and
long-term life prospects. It is important that pupils with SEND are
supported effectively so that they, as all children, achieve well in
their early years, at school and in college, and lead happy and
fulfilled lives.
The borough has a higher than average percentage of SEND pupils with
17.9% compared to 15.4% nationally, and 16.0% across statistical
neighbours . A key factor that differentiates SEND
provision in Wandsworth is the high number of children and young people
attending special schools who are not Wandsworth residents.
Wandsworth is home to a large amount of specialist provision,
including three regional special schools. This may explain why there are
more pupils with SEND being educated in the borough. 32.1% of pupils
attending state funded special schools live in another local authority.
This is considerably above the national average of 8.9%, and the London
average of 16.7% .
Wandsworth has the 2nd highest percentage of 0–24 year old
residents with EHCPs amongst statistical neighbours, and 32nd highest
among all local authorities putting it in the top third nationally . This
shows that despite out of borough residents forming a significant part
of the special school population, in terms of the Wandsworth resident
population with EHCPs, Wandsworth is still above average.
The large proportion of non-residents places a significant demand
on services in the borough and this needs to be considered as a local
priority. Taking account of all state funded schools (primary, secondary
and special), Wandsworth sits above the national average for the number
of pupils with SEND support.
In January 2020, 13.2% of pupils attending state funded schools
in Wandsworth were receiving SEND Support, compared with 12.1%
nationally and 12.4% amongst statistical neighbours. There are
variations across schools and between primary and secondary phases. The
percentage of primary school pupils with SEND support is 13.1%, similar
to the national rate of 12.8%. Support in secondary schools is 1.9%
higher than the national rate (13.0% vs 11.1%).
Furthermore, 2.8% of Wandsworth residents aged 0–24 years had an
EHCP compared with 2.3% nationally.
Wandsworth’s 2018 proportion of primary and secondary school
children with special educational needs was 17.3%, significantly higher
than England and London averages, and 4th highest in London.
The latest borough figure was 16.1% lower from year 2014, in
comparison with a 19.4% decrease in England’s rate over the equivalent
time period.
Pupils
with special educational needs (SEN): % of school pupils with special
educational needs: In 2022/23, Wandsworth’s rate was 19.7%
(n=8543), which was the 4th highest in London, 13.9% higher than the
England average and 18.7% higher than the London average. The latest
Borough figure for 2022/23 was also 13.9% higher than in 2015/16, in
comparison with 20.1% increase in England’s rate in the equivalent time
period.
Source: OHID:
Public Health Profiles
Source: OHID: Public Health
Profiles
Cross Border Movement
A large number of out of borough residents are accessing services due
to the high level of provision in Wandsworth. According to DfE data from
January 2020 on local authority cross border movement of special school
pupils resident in England, 30.7% of pupils attending state funded
special schools in Wandsworth live in another local authority,
significantly higher than the national average of 8.5%, and London
average of 16.5%.
For mainstream schools the equivalent figures are:
- 9% of those attending state funded primary schools in Wandsworth
live in another local authority, compared with 3.8% nationally, and 8.7%
in London
- 28% of secondary school pupils attending state-funded secondary
schools in Wandsworth live in another local authority, compared with a
9.3% nationally and 20.3% in London .
From this data we can see the local authority cross border movement
in London is generally much higher than it is nationally. However,
Wandsworth still sits above the London average. The data shows a
significant proportion (almost a third) of pupils attending state funded
special schools in Wandsworth are not residents in the borough.
Geographical variation may reflect differences in local approaches and
in the characteristics of local authorities . Wandsworth’s high
proportion of specialist provision is attracting residents from other
boroughs.
In 2020, there were 842 pupils attending Wandsworth’s special
schools, representing 2% of the total pupil population in Wandsworth.
This is higher than the 1% of the pupil population attending special
schools across statistical neighbours . This difference can
be accounted for due to the amount of specialist provision in
Wandsworth, including three regional special schools, providing places
for many children and young people resident outside the borough. There
are other factors accounting for increased numbers of children in
specialist provision. The local authority has been actively increasing
its specialist provision to meet the demand for local places, and to
meet parents’ expectations and preferences.
14.3 Predictive Risk Factors
In January 2020 over 1.3 million pupils in England were recorded as
having SEND. Whilst there are a variety of reasons why a special
educational need or disability may be prevalent in a child or young
person, there are a number of predictive factors for SEND:
- children can be born with a disability or special need due to
several maternity and birth related factors
- certain characteristics related to age, gender and ethnicity are
predictive of those being identified with SEND but they are not the only
causal features
- interrelation of social factors must be considered, particularly
regarding ethnicity where overrepresentation of certain ethnic groups in
the SEND cohort may be related to the misidentification of need,
cultural barriers and misunderstanding
- wider social determinants of health including the variation in
experience have been identified as the main factor influencing health
outcomes, with studies finding social determinants have more of an
influence on health than healthcare, behaviours and genetics
- social determinants are the conditions in which people are born,
grow, live, work and age and these determinants are a factor for health
inequalities - the unfair and avoidable differences in health status .
- there are also biological and social predictive factors in relation
to the prevalence of SEND.
Maternity and Birth
Recent years have seen an increase in maternal age. This is
associated with higher risk factors for conditions associated with
learning disabilities, such as Down’s Syndrome. Fertility rates for
women aged 40 years + increased by 1.3% nationally between 2016–17. In
Wandsworth this is particularly high with 101 women per 1,000 aged 35–39
years giving birth, compared with a 67.5 per 1,000 nationally, and 31
per 1,000 women aged 40-44 years giving birth, compared with 14.9 per
1,000 nationally .
The number of women having multiple births (two or more babies from
one pregnancy) can be a predictor for the development of SEND. The
multiple birth rate in 2017 nationally was 15.9 per 1,000 women. This
compares to 17.4 per 1,000 women in Wandsworth. Multiple birth
pregnancies are associated with a higher risk of stillbirth, infant
deaths and child disability .
Smoking during pregnancy increases the risk of complications such as
miscarriage, premature birth, a low-birth-weight baby and still birth .
According to 2016/17 published data 10.7% of women nationally smoke at
time of delivery. Premature babies are more likely to have a SEND, a
learning difficulty (such as dyslexia or autism), or a sensory
difficulty such as deafness or impaired vision that requires special
educational assistance. The severity of the problems depends on the
degree of prematurity. This risk of SEND associated with prematurity
declines steadily with gestational age up to 36 weeks. A baby born at 24
weeks of gestation is more likely to have a SEND later in life than a
baby born at 36 weeks. In this particular study it was found that babies
born at 24–27 weeks were 6.92 times as likely to have a SEND as those
born at 40 weeks.
Immunisation rates can also be a predictor for the development of
SEND. The World Health Organisation (WHO) set a target of 95% coverage
for vaccine-preventable diseases, including the combined measles, mumps
and rubella (MMR) vaccine, in order to target elimination or control.
Measles, mumps and rubella and other infectious diseases can lead to
serious long-term health implications, including the development of
SEND. According to 2018/19 data, the national average for MMR completion
(two doses) at age 5 falls below the WHO target at 86.4%. Wandsworth
sits significantly below the WHO target and the national average at
79.4%, slightly higher than the London average (76.3%) .
Gender and Ethnicity
Nationally, according to school data, more boys than girls are
identified as having SEND across all age groups. In January 2020, 24.9%
of male pupils had SEND compared with 11.8% for females. There is
evidence to suggest that ethnicity plays a part in children’s likelihood
of being identified as having SEND, with 16.0% of Black pupils
identified as having SEND in January 2020, compared with 16.4% of White
British pupils, 15.2% of mixed ethnicity pupils and 11.9% of Asian
pupils .
Analysis of ethnicity data from the Disabled Children’s Register
(DCR) and pupil census show the link between ethnicity and SEND.
According to this analysis, children and young people of Black, mixed or
other ethnicities are more likely to be identified as having SEND. In
Wandsworth, specifically, Asian or Asian British children are
underrepresented on the DCR compared with a Wandsworth 0–18 Asian
population (9% compared with an 11%, respectively). Black or Black
British and mixed children and young people are overrepresented on the
DCR (22% and 17%, respectively, compared with a 16% and 14% of the
Wandsworth 0–18 years population).
An Oxford University study on ethnic disproportionality in the
identification of SEND based on a 2016 school census found substantial
ethnic disproportionality in certain areas, with the majority remaining
apparent even after accounting for pupil background characteristics.
Marked disproportionality was found for the following ethnic groups and
SEND:
- Black Caribbean and Pakistani pupils are overrepresented for
moderate learning difficulty (MLD), Indian and Chinese pupils are
underrepresented for MLD
- Black Caribbean and Mixed White & Black Caribbean pupils are
substantially overrepresented for social, emotional and mental health
(SEMH) needs
- All Asian groups are substantially underrepresented for SEMH and for
autism spectrum disorder (ASD). Disproportionality was found not to vary
much across Local Authorities; however, some variation does exist, and
it is important for local authorities to identify where this is apparent
and to explore factors that may be associated with it.
Socio-economic Disadvantage
There is a strong link between poverty and SEND. Children from low
income families are more likely than their peers to be born with
inherited SEND, more likely to develop SEND in childhood, and less
likely to move out of SEND categories while at school. Households with
poor social determinants, for example, poorer early years’ experience,
low incomes and overcrowding and/or cold housing, are associated with a
higher prevalence of SEND. The proportion of children under 16 years
living in low-income families nationally is 17%, and Wandsworth is
similar at 17.2% .
Department for Education (DfE) statistics show a clear link between
SEND and children living in poverty. Eligibility for free school meals
(FSM) is an indicator of deprivation. In January 27.1% children and
young people who qualify for free school meals are much more likely to
have special educational needs or disabilities than children and young
people who are not eligible for FSM (12.5%).
The largest difference occurs with pupils with SEMH as their primary
type of need, where 34% of pupils with SEND Support and 43% of pupils
with an EHCP are eligible for FSM, compared with a 13% of pupils without
SEND .
In Wandsworth, 33% of pupils with SEND are also eligible for FSM,
compared with a 20% of the total Wandsworth pupil population. This
disparity is notable within the primary school population, as 32% of
primary school pupils with SEND are eligible for FSM compared with a 19%
of the total primary school population .
Furthermore, from conducting an internal analysis on SEND provision
(SEND, SEND Support, EHCP) and Income Deprivation Affecting Children
Index (IDACI) in the Wandsworth school population we can see that pupils
with a SEND are consistently more likely to be experiencing deprivation
than those without a SEND. This is most prevalent within the EHCP
population but can be seen across all three categories.
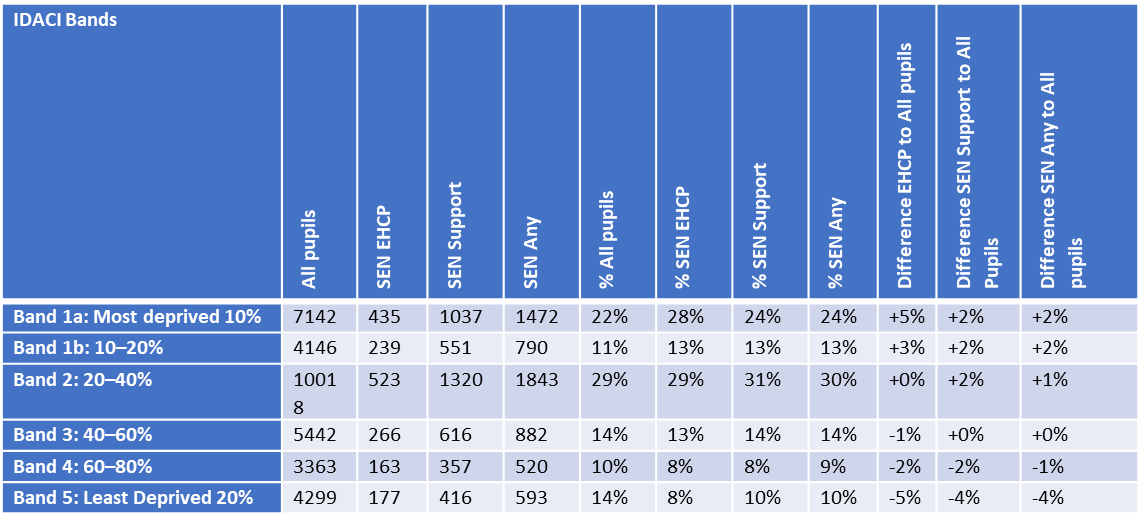
October School Census 2019 - SEND Provision and
IDACI in Wandsworth School Population
The Millennium Cohort Study showed that physical difficulties and
behavioural difficulties were particularly strongly associated with low
socio-economic status. Children living in poverty are more likely to
develop some forms of SEND, such as behavioural difficulties, as they
experience persistently challenging family circumstances .
Looked After Children / Children in Need
Nationally, looked after children have higher levels of SEND than
their non-looked after peers. The DfE has estimated that around half of
help or protection, including looked after children have SEND . The
incidence of SEND among looked after children and children in need in
Wandsworth in comparison to the national average for 2017–2019.
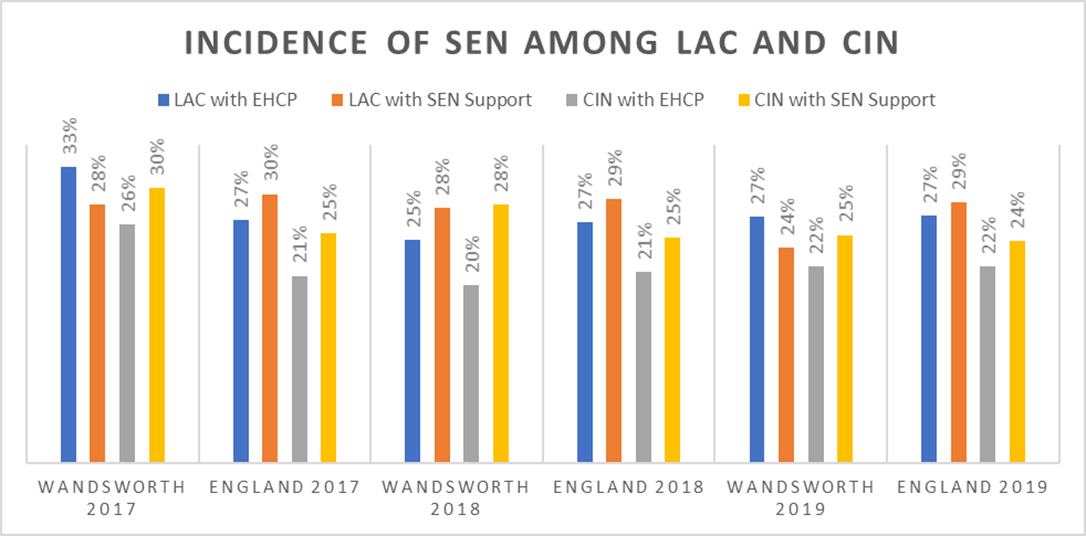
Incidence of SEND Among Looked After Children
and Children in Need in Wandsworth and England, 2017–2019
In July 2019, Wandsworth had a total of 305 looked after children. Of
this cohort, 42 children are recorded as having a disability (14%). In
May 2019, 179 looked after children were within statutory school age
(Reception to Year 11) and therefore open to the Virtual School. Of this
cohort, 93 (53%) have SEND needs, including 17% with an EHCP.
Involvement in Crime
A 2016 report from the Ministry of Justice and Department for
Education , those young offenders sentenced in 2014
(at the end of KS4 in academic year 2012/13) had a greater proportion
with SEND, when compared with the overall state-funded pupil population.
For all youth justice disposal types, behavioural, emotional and social
difficulties (BESD) was by far the most prevalent primary SEND type in
the matched cohort for those recorded with SEND. In 2019, 0.6% of the
0–25 years SEND resident population were known to the YOT service .
14.4 Education, Health and Care Plans (EHCP)
The total number of children and young people with an Education,
Health and Care Plan (EHCP) resident in Wandsworth was 2,418 in January
2020. This represents a 91% increase since the SEND reforms were
introduced in 2014 (1,265). According to the table below, Wandsworth
shows the 2nd highest increase in EHCPs amongst statistical neighbours
between 2016 and 2020. This represents a 91% increase since the SEND
reforms were introduced in 2014 (1,265). According to the table below,
Wandsworth shows the second highest increase in EHCPs amongst
statistical neighbours between 2016 and 2020.
In January 2020, 2.8% of Wandsworth residents aged 0–24 years had an
EHCP compared with 2.3% nationally, as per table below. Since 2016
Wandsworth has had a 73% increase in the number of residents with an
EHCP, compared to 52% nationally. Wandsworth has the 2nd highest
percentage of residents aged 0–24 years with EHCPs amongst statistical
neighbours, and 32nd highest among all local authorities .
The increase in volume of EHCPs is largely in the under 5 years,
16–19 years, and 20–25 years age groups. The increase in the older age
groups can be attributed to government policy to raise the age of EHCPs
to 25 years. It included those in college who had previously had a
Learning Difficulty Assessment (LDA) rather than a Statement of SEND. An
increase in primary aged pupils with EHCPs is in excess of any increase
that may be anticipated due to population changes.
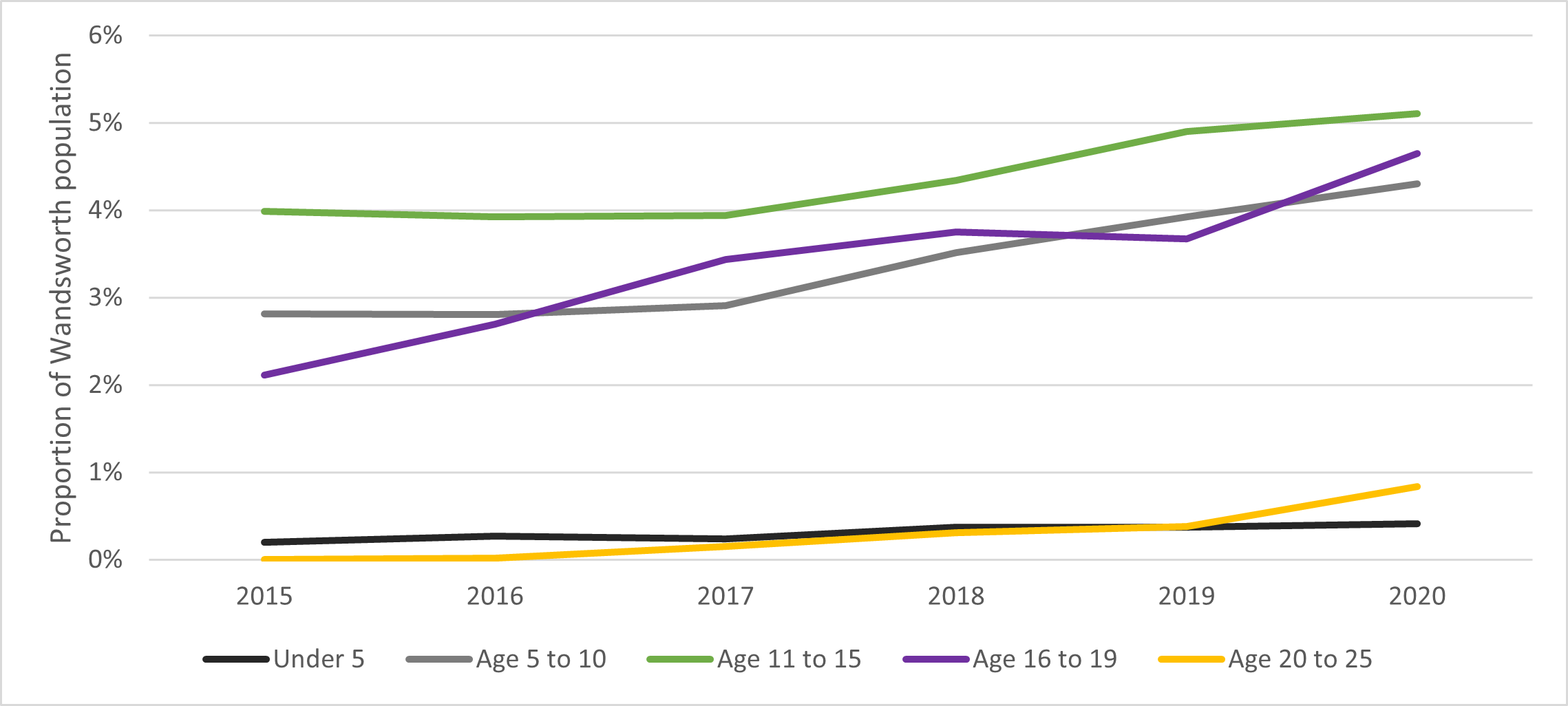
EHCPs as a Proportion of the Population in
Wandsworth, 2015–2020
Source: Population projection Estimates from GLA data February 2020
and EHCP figures from SEN2 SFR
72% of children and young people in the borough with EHCPs are male,
30% are female. 69.6% with EHCPs are from a Black Asian and Ethnic
Minority background. The largest (minority) group are Black or Black
British, accounting for 25.5% of children and young people with EHCPs . This
shows that whilst Wandsworth has a high proportion of EHCPs, there is a
significantly high level of need amongst males and those of Black
ethnicity.
The high proportion of males with EHCPs is a common trend at a
national level. Higher prevalence in young males may be due to
biological vulnerability to disability that affects their learning,
either from birth or as they develop. More young males experiencing
difficulty with their education are identified as having SEND than young
females, due to their propensity to act out and display hyperactive,
impulsive, or disruptive behaviour .
Another measure of need in is the number of people in receipt of
Disability Living Allowance (DLA) or Personal Independence Payments
(PIP). This is a slightly different cohort of people as some of these
people may not have an EHCP. The number of young people in receipt of
DLA or PIP has increased by 34% from 1,920 in 2011 to 2,566 in 2018. In
2019 there were 1,849 children aged 0-15 years, and 192 young people
aged 18-24 years receiving DLA. In April 2019 there were 637 young
people aged 16-24 years in receipt of the PIP.
The number of adults aged 18-24 years with learning disabilities in
Wandsworth is projected to increase by 17% from 681 in 2017 to 799 in
2035. The prevalence of learning disabilities among this age group is
predicted to grow more rapidly than all other age groups. The total
number of adults with learning disabilities aged 18-64 years is
projected to increase by 9% over the same period. This has implications
for the level of demand with regard to EHCPs in the borough, as well an
increasing level of need in the 18–24 year olds.
SEND Support
In January 2020, there were 5903 pupils with SEND in Wandsworth,
13.2% of all pupils. This number is slightly up from 5741 (12.8%) in
2019 but has remained with 5842, (13.4%) in 2016 . Wandsworth has a
slightly higher proportion of pupils on SEND Support than the national
average of 12.1%. There is significant variation in these figures
amongst schools, some may be due to over identification of SEND.
According to the latest school census data (January 2020), pupils with
SEND Support were nearly twice as likely to be boys than girls (64%
compared with a 35%).
14.5 Prevalence of Areas of Need
The prevalence of different types of need nationally is measured
annually by the DfE. Data collections report on the primary needs of
pupils with special educational needs and/or disability within
state-funded schools. Changes and disparities in diagnostic practices
over time mean that longer term trends are less reliable. Key trends
from national data set include:
- a reduction in the proportion of pupils with specific learning
difficulties and moderate learning difficulties
- an increase in the proportion of students with autistic spectrum
disorder since 2015
- an increase in the proportion of students with speech, language and
communication needs since 2015.
These trends are also visible in the Wandsworth dataset. The decrease
in pupils with moderate learning difficulty (MLD), and the increase in
pupils with autism spectrum disorder (ASD) are more pronounced. These
datasets only indicate the primary need, a shift from MLD to ASD does
not preclude co-morbidity.
As shown in the table below, the most prevalent primary types of need
in Wandsworth are speech, language and communication needs (SLCN) at
26.7%, SEMH at 20.4% and ASD at 13.8%, above the England average for all
three categories.
Source: PANSI LD – Baseline estimates
The Family Resources Survey (FRS) captures
prevalence data regarding the different types of impairment that
children aged 18 years and under have in the UK. Data from this survey
cannot be compared directly with Department for Education (DfE) data as
the age ranges are different. The FRS allows for multiple impairments
whereas the DfE data only includes primary types of need, using
different classifications. However, both surveys indicate similar trends
including:
- sensory and physical needs are becoming less prevalent, most notably
stamina, breathing, fatigue and hearing impairments
- the prevalence of social and behavioural needs has increased by 24%
since 2012/13
- the prevalence of learning disabilities has increased by 19% since
2012/13.
Hearing, Visual, Multi-sensory Impairments
Despite data suggesting decreasing prevalence in sensory and physical
needs in the UK, Wandsworth has the highest proportion compared with the
statistical neighbours of pupils with hearing impairments, 3.1% compared
with 1.8% nationally. The incidence of visual impairments in Wandsworth
is 2.3% compared with 1.0% nationally. The number of pupils with
multi-sensory impairments as their primary need is 0.6% compared to 0.3%
nationally. Wandsworth is also the second highest nationally for the
proportion of pupils with visual impairments Table 12.
Wandsworth has two specialist schools, two resource bases and a
sensory support service for these types of impairments which might
explain the significant proportion of pupils in comparison with national
and statistical neighbours. Nevertheless, it represents a high level of
demand which must be met by the local authority.
Autism Spectrum Disorder (ASD)
In 2020, 13.8% of pupils with SEND had ASD as their primary need
compared with 11.9% nationally. Since 2016 there has been a 3.6%
increase in the proportion of the school population with ASD as their
primary need compared with a national increase of 3.1%. The increase in
prevalence is not unique to Wandsworth. In common with other local
authorities, Wandsworth is experiencing a significant growth in children
and young people identified with ASD receiving services from 161 in 2001
to 1406 in 2018/19. There are now more than 1 in 50 children aged
between 7-15 years identified with ASD and receive specialist services.
This is significantly higher than rates quoted by the National Autistic
Society of about 1.1 in 100 , representing a significant level of
need in the borough.
In light of the increasing ASD diagnoses and consequent significant
impact of demand for assessments, intervention services, and special
school places, a review of the ASD Pathway in Wandsworth was conducted.
It found that parental satisfaction with the level of support and/or
training offered was largely below 50%.
63% of parents answered that they had come across difficulties when
accessing support services, notably long waiting lists for therapy
services, the inflexibility of training courses, and difficulty in
accessing CAMHS support. Following consultation on restructuring the
pathway, which was largely supported by respondents, proposals were put
forward to and agreed by the Council Executive in July 2019. Proposals
are being implemented, with changes reflecting the concerns raised
during the consultation phase. The impact of this is yet to be seen.
There is a Designated Medical Officer for the area, who has been
closely involved with the review of the ASD pathway. The Special
Education Needs and Disabilities (SEND) Code of Practice, states that
partners “should ensure that there is a Designated Medical Officer (DMO)
to support the CCG in meeting its statutory responsibilities for
children and young people with SEND”. A service review was conducted
into the role of the DMO due to increased demand on the role. Extra
capacity has been provided but it is yet unclear whether this is
sufficient to meet current demand.
Despite evidence of increasing ASD diagnoses, a study conducted by
the National Autistic Society on challenges for families affected by
autism in Black, Asian and Minority Ethnic communities found that
families reported experiences of misdiagnosis or no diagnosis This was
often because the child was just thought to have behavioural
difficulties rather than ASD .
Social, Emotional and Mental Health Needs (SEMH)
As of January 2020, the proportion of pupils with SEMH in Wandsworth
as their primary need is 20.4% of the total SEND population. This is
above the national average of 17.8%. Wandsworth schools have the 21st
highest proportion of pupils with SEMH nationally:
- within state-funded primary schools the proportion is 18.8% in
Wandsworth, compared with a 15.3% in London and 16.8% nationally
- within state-funded secondary schools the proportion in Wandsworth
is 25.9% compared with a 20.8% in London and 20.7% nationally
- within special schools the proportion in Wandsworth is 12.4%
compared with an 8.7% in London and 12.8% across England .
According to the local authority report for Wandsworth as part of the
study on ethnic disproportionality in the identification of SEND, the
Wandsworth unadjusted data showed Black Caribbean pupils were over four
times as likely to be identified with social, emotional and mental
health (SEMH) needs than the White British majority. They are also being
overrepresented for Specific Learning Difficulties (SpLD), Moderate
Learning Difficulty (MLD), Speech, Language and Communication Needs
(SLCN), Autism Spectrum Disorder (ASD) and for any SEND. Whilst Black
Caribbean pupils were generally overrepresented nationally, Wandsworth
shows a particularly high level of overrepresentation .
The adjusted data (accounting for factors such as socioeconomic
disadvantage, gender, birth season and year group) shows that Black
Caribbean pupils were still two and a half times as likely to be
identified as having SEMH needs than the White British majority and
shows overrepresentation for all the aforementioned categories of SEND.
Wandsworth showed the highest SEMH incidence in Black Caribbean and
Mixed White and Caribbean of all local authorities nationally at 11.5%.
Wandsworth also showed the 3rd highest incidence of any SEND in Black
ethnic groups at 24.5%.
One proposed explanation for the overrepresentation of Black pupils
with SEMH/MLD is inappropriate interpretation of ethnic and cultural
differences. Alternatively, the disproportionality may reflect ethnic
minority pupils experiencing substantially greater socioeconomic
disadvantage relative to the White majority .
The findings for Wandsworth of the recently published study show that
over-identification of SEMH among pupils from Black Caribbean and Mixed
White and Black Caribbean ethnicities cannot be wholly explained by
other factors associated with high levels of SEMH (e.g., deprivation,
socioeconomic disadvantage), suggesting that racial biases may be
leading to the over-identification of this type of need amongst this
demographic. There are long term trends indicating that some schools
over identify this type of need and this will need be monitored on an
ongoing basis . These disparities reflect wider
research that has demonstrated links between certain types of need and
ethnicities across local authorities nationally, which may be reflective
of misidentification of need.
This evidence makes clear that there is a danger that ethnic
disproportionality, if not addressed, may lead to inadequate or
inappropriate provision, and perpetuate unequal outcomes.
Speech, Language and Communication Needs
In Wandsworth, 30.8% of SEND Support pupils had speech, language and
communication needs as their primary need, compared with a 23.7%
nationally .
Nationally, of those pupils with speech, language and communication
needs, 25.9% of them have a first language other than English (January
2020) . In Wandsworth, as calculated
internally using the January 2020 school census, this is almost double
at 49.1%. However, it should be considered that Wandsworth has a much
higher percentage of pupils who are classified as having English as an
additional language (EAL) with 43.4% in primary schools and 42.5% in
secondary schools, compared with a 21.2% and 16.9% nationally.
It is important to note that when a child who is learning English as
an additional language makes slow progress in school, it is sometimes
difficult to tell whether the delay is caused because they are not
confident using the language or because they have a specific learning
difficulty independent of the language. Educational psychologists
provide an essential role in the assessment of the distinction between
language learning needs and special needs.
As schools record needs, schools must be mindful of how they record
speech, language and communication needs in EAL pupils to make sure that
it is an actual need each time. The importance of being able to
discriminate clearly between the need for EAL support and the need for
SEND Support is readily acknowledged by teachers. But it is also widely
recognised that, in practice, distinguishing between a language learning
need and a special educational need is a difficult task . The SEND Code of
Practice recommends that very careful consideration be given to the
identification and assessment of the special educational needs of pupils
whose first language is not English. It highlights the need to consider
the context of the home, culture and community and, where appropriate,
take advantage of any local sources of advice and liaison arrangements
within the relevant ethnic community.
Lack of careful consideration may lead to misidentification of need
or misdiagnosis by assuming the child has a learning difficulty as
opposed to a language or cultural barrier. Assumptions about a child’s
expected language ability may also delay diagnosis. It may be
interpreted a child’s delayed development and speech is due to them
speaking another language.
Attainment – Education, Employment and Training
Generally, in Wandsworth there is evidence of good educational
outcomes for those on SEND Support. However, positive outcomes are not
always shared among those with EHCPs. In 2019, 37% of the pupils
receiving SEND Support achieved the expected standard in reading,
writing and maths at the end of Key Stage 2. This is significantly
higher than the national average of 25%, and the statistical neighbour
average of 36%. For those with an EHCP however, only 6% reached the
expected standard, lower than the national average of 9%, and
statistical neighbour average of 13% . However, as
Wandsworth has a higher proportion receiving SEND Support, one could
assume a possibility that these good results may in part be due to an
overidentification of need.
Issues concerning timeliness of issuing new EHCPs could be a cause of
lower than average attainment. The 0–25 year old SEND Code of Practice
states the whole process of EHC needs assessment and EHCP development,
from the point when an assessment is requested (or a child or young
person is brought to the attention of the local authority) until the
final EHCP is issued, must take no more than 20 weeks. In Wandsworth in
2019, 45.4% of new EHCPs were issued within the statutory 20 weeks .
EHCP timeliness remains an ongoing issue across many local authorities.
Nationally the number of EHCPs issued within 20 weeks fell from 64.9% in
2017 to 60.4% in 2019.
There have been significant improvements in Wandsworth since 2015
when the achievement rate was 28.7%. However, the current rate still
sits below this national average as well as our statistical neighbour
average of 74.1%. This will continue to be a priority for the
Council.
Looking at the outcomes of the EHCP cohort resident population in
January 2019, the percentage of children and young people with EHCPs
attending post-16 institutions in Wandsworth was 10.4%. This is below
national (16.2%) and London (13.6%) averages . The percentage of
19 year olds in 2018 with a statement or EHCP qualified to level 2
including English and maths (14.1%) was below the London average
(16.4%), and the national average (14.8%) . However, the
proportion of young people with EHCPs who were not in education,
employment and training (NEET) improved in 2018/19 and is now better
than average as 4th highest amongst statistical neighbours, and 19th
highest nationally.
Absence and Exclusions
There is a relatively high percentage of persistent absentees in
special schools in Wandsworth, at 30.7% compared with 30.1% statistical
neighbours, and 28.1% England . This is a dramatic decrease from 35.4%
in 2018. It is important to note the definition of persistent absence
used by the DfE is “pupils missing 10 percent or more of their own
possible sessions (due to authorised or unauthorised absence) are
classified as persistent absentees”. This means children who are
frequently too unwell to go to school (authorised absence) are counted
in this measure. It may be interesting to see what proportion of
persistent absences have an impact on the inflated figures (table
below).
The fixed-term exclusion for the academic year 2018/19 across all
schools in Wandsworth was 6.2% for SEND Support pupils, and 7.6% for
those with an EHCP, down from 7.1% and 9.6% respectively in 2017/18.
Wandsworth now has the lowest rate amongst statistical neighbours.
Despite this, we are aware of children who have been off-rolled and who
are on reduced timetables require attention.
As shown in the table below, fixed term exclusion rates for pupils
with SEND are considerably higher than for pupils with no SEND and have
increased from the previous year in all categories. These figures are
much lower than the national average. The fact that pupils with SEND are
consistently excluded more often than their peers needs to be addressed,
particularly to see if they can be given more support which may help
keep them in school.
Both for EHCP and SEND Support, it is notable the rate of pupils who
have had at least one fixed term exclusion is lower in Wandsworth than
the national average. In 2018/19, the permanent exclusion rate for both
EHCP and SEND Support pupils was lower in Wandsworth than
nationally.
Transition to Adulthood
In 2020, according to data held within the Disability Team for 0–25
year olds, there are 144 0–17-year-olds and 192 18–25-year-olds in the
service. The considerable projected increase in number of adults aged
18-24 years with learning disabilities means there could be more demand
on transition services in the coming years.
All young people within the 0–25 years Disability Team are eligible
for an assessment under The Care Act (2014) . A transition
assessment is carried out where it is likely the young person will have
care or support needs after they turn 18 years old. This is highly
likely to be the case where the young person is currently in receipt of
children’s services for their disabilities. For young people with SEND
the assessment should inform a plan for the transition from children’s
services to adult care and support.
Those young people outside of the 0–25 years team, for example
managed by other teams in children’s services, children in need or
looked after children, are referred to the Transitions Panel so that
their pathway can be planned jointly by Children’s and Adults’ Services.
The Transitions Panel service has recently been reconfigured leading to
challenges in performance tracking including predicting future needs at
18 years old. This is being addressed as a priority. The identification
of SEND also appears lower than expected for those that are subject to
child protection plans. This has led to a higher than expected referral
rate to the Transitions Panel.
Transition planning for care leavers with complex needs into adult
services continues to be a challenge with some young people not
receiving the support they need in a timely or well-planned manner.
Under the Care Act 2014, and Section 16 of the Statutory
Guidance , the CCG is required to support the
local authority in the transition to adult services. Children’s
Continuing Care must alert the appropriate services when the young
person is at the age of 14 years and a decision should be put in place
in principle by the age of 17years so that Adults’ Continuing Healthcare
commences immediately when the young person turns 18 years old.
Transition planning at the age of 14 years is challenging to achieve due
to high demand, can lead to additional pressures on Adult’s Continuing
Healthcare, and disruption in packages of support. Entitlements for
under 18 years for support is often greater than that provided by Adult
Services.
A Transitions Officer role created within CAMHS has the principal
responsibility of strengthening transition pathways into adult services.
Transitions are also supported through the local authority contacting
parents and carers with children on the Disabled Children’s Register
(DCR). They inform them of the transitions process well in advance of
their 18th birthday. This has proven to be very effective as there is
evidence of a peak in referrals in the months when letters are sent.
Unidentified and Unmet Areas of Need
Part of addressing need is identifying areas where there are
unidentified needs amongst children and young people. There are however
processes in place, or being put into place, which may help us to
identify this unmet need in children and young people with SEND. For
example, the Disabled Children’s Register can be used to capture areas
of need. It collects information on children and young people in the
borough with a physical or learning disability which can be used to help
the local authority with the identification of needs.
There are other areas of need listed below:
Children and Young People with Attention Deficit and Hyperactivity
Disorder (ADHD)
One of the categories of need which is not being met sufficiently
being met is children and young people with attention deficit
hyperactivity disorder (ADHD). One of the main issues is that ADHD is
not recorded as a primary need, instead being recorded under the primary
need of SEMH or ASD. This can lead to unmet need because the services
and support provided for children and young people with SEMH, ASD or
ADHD may be quite different. Furthermore, as ADHD is not recorded as a
primary need, the exact number children and young people with ADHD is
unknown. There is also an impact on education as we are aware that many
pupils diagnosed with ADHD are not in schools, may have been excluded or
are in a Pupil Referral Unit (PRU), finding it hard to get a place back
in a school. According to latest national school census data on
attendance for the academic year 2017/18, pupils with SEMH needs account
for the 2nd highest proportion of overall absences at 9.3%, the highest
proportion of unauthorised absence of any category. Furthermore, pupils
with SEMH account for the 3rd highest proportion of persistent absentees
at 27.6% (table below).
The fact that ADHD is not recognised as a primary need in itself,
means that children and young people with ADHD are potentially not
getting enough of the right type of support, which not only affects
their health, but can have an impact on their education. Further
consideration must be given to the specific support required by these
children and young people.
High-functioning Autism Spectrum Disorder (ASD)
There is a significant proportion of children and young people with
high-functioning ASD who are out of school or are educated in
independent placements, due to their anxiety, SEMH or ADHD needs. The
fact they are unable to attend mainstream secondary schools suggests
there is an unmet need.
School Absenteeism
One of the potential explanations for high and persistent absentee
levels in special schools may be because authorised absences are for
those who are too unwell to go to school. Some children in specialist
provision are frequently too unwell to go to school, whether this be
mentally or physically. Medical needs can impede school attendance and
affect educational attainment. There is a potential gap in relation to
providing education at home.
Mental Health Support Process/Care, Education and Treatment Reviews
(CETR)
CETRs are focused on those children and young people who have either
been or may be about to be admitted to a Specialist Mental
Health/Learning Disability Hospital. CETRs are not always conducted
which means health needs are not addressed as a consequence of problems
and delays in the process.
SEND Support Guidance
Many local authorities have produced guidance on SEND Support within
schools. Wandsworth guidelines on SEND support are being reviewed as
part of the SEND Support subgroup of the SEND Strategic Partnership
Board Of course, all schools are different and there is variation in the
number of pupils with SEND Support across schools. As laid out in Part 3
of the Children and Families Act 2014, a child or young person has SEND
if they have a significantly greater difficulty in learning than most
others of the same age. In some schools, quality-first teaching means
schools can manage need and therefore is representative of a low level
of SEND Support, whereas in other schools there may be a particularly
high proportion of pupils receiving SEND Support, potentially due to
overidentification. Some clearer consistency on what is generally
classed as a special educational need may benefit schools to combat
instances of over- or under-identification.
14.8 Current Services and Good Practice
Children and young people with SEND and their families face distinct
and challenging issues that require a range of dedicated and specialist
responses from public services. The full range of local services is
detailed on Wandsworth’s Local Offer website. The aim of the website is
to provide advice and information of the range of services and options
available for children and young people with SEND. Below is a list of
available of support services:
Annual Health Checks
Annual health checks for people with learning disabilities have been
introduced to reduce health inequalities. Anyone aged 14 years or over
who is on their GP’s Learning Disability Register can have a free health
check once a year. You can ask to go on this register if you think you
have a learning disability, you do not need to be diagnosed with a
learning disability. All GP surgeries in Wandsworth offer annual health
checks if there is evidence of a learning disability.
Autistic Syndrome Disorder (ASD) Pathway
Currently ASD assessments are led by paediatricians at St George’s
Hospital when a child is below the age of 8 years, and by clinical
psychologists from specialist CAMHS services when a child is older than
8 years. The child is then referred to specialist services where
appropriate, and parents are signposted to support and training.
A review and refresh of the ASD pathway has been conducted to ensure
service models for assessment, diagnosis and intervention are effective
across the age range. The review aimed to clarify waiting times and
active early interventions offered prior to full diagnostic assessment,
including piloting new approaches to triage and support.
CAMHS Access Service
South West London and St George’s Mental Health Trust are
commissioned by Wandsworth CCG to deliver the CAMHS Access Service. It
acts as a single point of access to CAMHS for children and young people
up to the age of 18 years who are registered with a Wandsworth GP.
The local authority provides Access Family Consultancy as part of
this service. These are joint sessions where young people, their parents
and carers can identify and discuss which issues are having an impact on
their family well-being.
CAMHS Plus
CAMHS Plus supports the transition from child to adult mental health
services for young people aged 18 years and over. Transitions across the
system of care is a significant and essential component of the
transition planning process for young people who are involved with
multiple agencies across the health, education and social care
sectors.
CAMHS Under 5 Service
The local authority commissions a CAMHS Under 5 Years Team who are
embedded in children’s centres and work closely with health visiting and
GP services. The service offers 1-2-1 and group sessions to under 5 year
olds and their families. Referrals can be made by GPs, health visitors,
nurseries and other professionals working with the children.
Child Development Centre at St George’s Hospital
The Child Development Centre (CDC) has specialist services such as
physiotherapy, psychology, and speech and language therapy, paediatric
neurodevelopment, neurodisability and epilepsy services. These services
run clinics at St George’s Hospital, and provide outreach services at
regional hospitals or centres such as the Early Years Centre.
Children’s Occupational Therapy Team
The children’s occupational therapy service is focused on enabling
children aged 0-11 year olds to participate in daily activities to
improve their independence and well-being. The service works with
children who are unable to do daily occupations due to illness,
disability, family circumstances, or as a result of changes as they get
older. The service can provide assessments and advice if access to
certain buildings or places in the community is problematic, and it
assists and advises schools on ensuring their facilities are accessible
for children with disabilities.
Disability Access Fund
The Disability Access Fund is available for children aged 3 or 4
years old in receipt of Disability Living Allowance (DLA). It is a
one-off payment of £615 to the provider for resources, equipment and
adaptations which improve inclusion.
Early Support
The Early Support Service assists the families of children aged 0-5
years old with complex medical needs through an assisted or designated
key working stream. Assisted support involves regular check-ins with a
member of the team and the opportunity to access drop-in sessions. A key
worker is assigned to the family and liaises with professionals
supporting the child to arrange the Team Around the Child (TAC) meetings
or assist with appointments and home visits.
Early Years Speech and Language Therapy Service
The Council commissions a Speech and Language Service to undertake
early identification and therapeutic support through children’s centres.
The service is designed to be flexible and comprehensive so that the
therapist sees a child and their family at the right time, in the most
appropriate setting.
Educational Psychologists
Educational psychologists are part of the Schools and Community
Psychology Service (SCPS) service listed above. They work with children
aged 0–25 years who may need SEN Support or are placed at SEND Support
(if school age) as part of an education, health and care needs
assessment (EHCNA), or those who have EHCPs.
Get Set Go
Following consultation with young people, Get Set Go was set up by
Wandsworth Council and South Thames College as a forum to showcase
opportunities for employment, education, training and independent
living. These events take place annually to support young people aged 14
-25 years in preparing for adulthood.
Health Visiting Service
The Health Visiting Service has been provided by CLCH since January
2018. It provides a universal support and advice service to all
Wandsworth resident children aged 0-5 years old and their families. They
promote health, assist in the early identification of development and
health needs, prevent accidents, and ensure immunisations are completed.
They also run a targeted health visiting service for children and
families who require extra support. This service assesses each child and
family and introduces them into appropriate services, such as speech and
language therapy.
Mainstream Schools and Resource Bases Speech and Language Therapy
Service
The school age service provides an assessment and intervention
service for children in Reception and Years 1 to 11 in Wandsworth
maintained schools. Every mainstream school within the Borough has a
named speech and language therapist. The therapist provides support and
therapy to children in school settings and educates staff to provide
intervention guided by a speech and language therapist or speech and
language therapy assistant (SLTA) and use strategies recommended,
modelled and explained by the speech and language therapist. Three
resource bases within the borough also commission the service
(Smallwood, Tooting and Southmead). Speech and language therapists are
located within these resource bases working closely with the staff and
children.
Mental Health Trailblazers
Mental health trailblazers are being developed as part of the
government agenda to tackle mental health needs in children and young
people. This involves establishing new Mental Health Support Teams to
develop models of early intervention, and to support staff in schools
and colleges. There is a trailblazer in a cluster of schools in
Southfields and a new one developing across a Battersea cluster. South
Thames is also part of a further education college trailblazer.
Paddock School Based Therapy Team
The Paddock School Therapy Team takes an integrated approach to
therapy and learning with the class team, families, and therapists,
working together to set joint goals. The service aims to enhance future
provision by expanding the range of tools being used to capture the
pupil’s voice including observation of behaviour, talking mats,
inclusion and belonging surveys.
PATHS
Promoting Alternative Thinking Skills (PATHS) is an evidence-based
programme which takes place in the most deprived schools in Wandsworth.
The programme helps reduce incidents of aggression and violence and
exclusions.
Personal Budgets
The SEND reforms have enabled greater personalisation of support
including the use of a personal budget. Children, young people and their
families have greater choice and control over the design of the health,
social care and education package. The personal SEND budget is a sum of
money made available by the local area at the request of a parent or
young person. It is allocated on the basis it would not be possible to
meet the child’s needs without additional funding.
Place2be
Place2Be services are commissioned by Wandsworth CCG, operating
within primary schools in Wandsworth. They deliver a range of services
for 5-11 year olds including 1-2-1 counselling sessions, group work,
teacher training, parental support and Place2Talk lunchtime sessions.
Place2Be’s aim is to deliver therapeutic services that meet the
emotional and behavioural needs of children and improve their
well-being.
Portage Service
Wandsworth Portage is a home-based early education service for
pre-school SEND children and their families. Portage provides weekly or
fortnightly visits to provide activities and ideas to help each child
develop. It supports parents to monitor their child’s progress and
development as well as providing them with emotional and practical
support. It also assists with transitional arrangements as the child
approaches school age. The team collaborates with therapists, health
visitors and educational psychologists, to develop activities to
stimulate each child’s development.
Pre-School Specialist Speech and Language Therapy Service
This service is a Specialist Assessment and Therapeutic Service
working with children with complex developmental and communication
needs. Children receive intervention from 2 years until the term they
start school. However, children are seen up to 8 years of age as part of
a multidisciplinary assessment for possible autistic spectrum disorder.
Children are seen within a range of clinical settings as well as their
nurseries and schools. Speech and language therapists work with children
with a hearing impairment up to the age of 18 years.
Resource Bases
The Council has worked collaboratively with a range of schools to set
up bases to meet the needs of the increasing number of children and
young people diagnosed with ASD, as well as existing speech, language
and communication needs, MLD and hearing-impairments. It has also
collaborated with South Thames College to open a base for pupils aged 19
years + with complex needs (Aurora) at its Merton Campus. There are
currently 16 resource bases in the borough.
Wandsworth Autism Advisory Service
The new Wandsworth Autism Advisory Service works closely with
partners across the authority to provide a planned and graduated support
to parents and families of children with a diagnosis of autism, and
those on the specialist pathway. The service provides specialist advice
and support for parents and will upskill families through a bespoke and
differentiated parent and carer training programme.
Wandsworth Sensory Support Service
Wandsworth Sensory Support Service (WSSS) caters for children and
young people who have hearing and visual impairments, as well as those
with complex needs. WSSS comprises Linden Lodge School and Wandsworth
Hearing Support and Vision Support Services.
WAND/Wand+ Card
The WAND Card Scheme was introduced in 2013 to increase the
proportion of children registered on the Disabled Children’s Register
(DCR). The WAND Card can be used as a form of ID for children with SEND
and allows access to a number of offers with local businesses and
services. The WAND+ card is for young people aged 18-24 years old with
special educational needs, disabilities or complex health needs. Full
details of the offers, events and deals for WAND card holders can be
found on the Local Offer website.
Specialist Youth Services
As well as a range of Youth Clubs which welcome children and young
people SEND, the Council commissions youth Groups in Wandsworth
specifically for young people with SEND. They include the Unique Youth
at the George Shearing Centre, Generate, the Lady Allen Playground and
Baked Bean.
Speech and Language Therapy ‘Talk Shops’
Parents and carers can self-refer to this service, and open access
drop-in sessions are run regularly within children’s centres. A basic
assessment may be conducted during these sessions and children can be
referred for a full assessment. Parents are provided with age
appropriate advice, support and information. For 0–3-year-olds, “Support
for Little Talkers” workshops for parents have also been introduced.
Schools and Community Psychology Service (SCPS)
The SCPS delivers a number of different services across education,
health, and social care settings to promote the positive development and
well-being of children and young people. Consultation, advice,
assessment and intervention are offered on:
- children’s learning and development
- social and emotional needs and behaviours
- psychological well-being and mental health
- parenting.
The service works with children, young people, their families,
schools and other professionals, using applied psychological theories
and approaches to analyse and help make sense of real-world situations
and complex problems, and ensure a coordinated approach. The service has
expertise in research, evaluation, training and supervision. It also
offers critical incident support to schools when there has been a
significant event affecting the emotional well-being of pupils and
staff.
Supported Internships
Supported internships are a structured study programme based
primarily with an employer. They are unpaid and last for a minimum of
six months, and normally for a year. They are usually 20 hours per week.
Wherever possible the young person will be supported to move into paid
employment at the end of the programme. Alongside their time with the
employer, young people complete a personalised study programme which
includes the chance to study for relevant substantial qualifications and
English and maths.
SEND Inclusion Fund
The SEND Inclusion Fund is available to ensure that 3 and 4 year old
children with additional needs can participate fully in activities in
early education settings. The fund is payable directly to providers.
Additional needs may include a physical, sensory or learning disability,
or difficulties in areas such as communication, attention and
behaviour.
Short Breaks
Short Breaks give parents and carers of SEND children and young
people the chance to have a break from their caring responsibilities.
The local area offers a wide range of short breaks for children with
disabilities, ranging from support for families to spend time together,
to targeted support (wherever possible accessed without the need for an
additional assessment), through to specialist services accessed through
a social work assessment.
Special Schools
Wandsworth Borough Council maintains five special schools, three of
which are regional providers with residential provision catering for
children from across London and Southern England. A sixth school
(Nightingale) became an Academy in October 2016 as part of the Orchard
Hill College Academy Trust. Linden Lodge became an academy, with the
Southfields Multi-Academy Trust in September 2018.
Specialist CAMHS Service
This is a multi-disciplinary service providing a specialised service
for children and young people with severe, complex and persistent mental
health disorders. It provides a comprehensive Tier 3 assessment and
treatment service.
Travel Assistance
A variety of travel assistance is provided for some children with
EHCPs whose and includes mileage reimbursement, personal travel budgets
and travel training. Travel Assistance Budgets (TABs) allow parents and
carers to independently arrange the best way to get their child to
school, in a way that is convenient for them. The provision of travel
training enables the development of young people’s skills and confidence
to use public transport and allows them to become more independent.
Travel training is available for secondary aged young people who have
been assessed as being ready and able to begin learning to travel to and
from school independently.
Wandle Early Years Hub
Young people in Merton and Wandsworth benefit from an Early Years
Hub, funded by the Mayor of London’s Office. The Wandle Early Years Hub
is one of only three across London. It works to improve the take up of
free provision for eligible 2 year olds, improve provision for the most
disadvantaged children, and improve early intervention for children with
SEND.
West Hill Enhanced Children’s Centre
The Enhanced Children’s Centre is a specialist setting supporting all
families in Wandsworth with children aged 0-5 years old with a
disability, special or complex medical need. The centre provides
services to children aged 0-5 years and their families including play
and learning sessions, therapy sessions and parent groups. The centre
works closely with professionals and therapists, and CAMHS workers can
use the centre to run drop-in sessions or targeted programmes of work.
They run programmes on topics such as parent well-being, sleep,
behaviour, feeding and sensory needs.
Workright
The Council employs a dedicated employment coordinator to liaise with
local employers to develop supported employment and internship
opportunities.
Youth Offending Team Screening & Assessment
All young people attending the Youth Offending Team are initially
screened and assessed for speech, language and communication needs
(SLCN), provided they have given their consent to pick up previously
unidentified needs. A key challenge is differentiating mental health
needs from SLCN.
14.9 Evidence Base and Good Practice
Early identification and intervention have been identified as crucial
to improving the health and well-being of children and young people with
SEND.
NICE Guidance implementation
NICE guidance on transition from Children’s to Adults’ Services
includes recommendations on planning and carrying out transitions to
help young people and their carers have a better experience of
transition.
Key recommendations include:
- involving young people and carers in service design, delivery and
evaluation related to transition
- ensuring transition support is developmentally appropriate
- strengths-based transition support (focus on what is positive and
possible for the young person rather than a predetermined set of
transition options)
- adoption of a person-centred approach
- integration between health and social care managers in Children and
Adult Services
- planning for adulthood from age 13/14 years at the latest
- identification of a named worker for each young person to coordinate
their transition
- local, integrated youth forums to provide feedback on existing
service quality, and highlight any gaps
- preparation for transition should start early.
As stated in the SEND Code of Practice, “When a child is very young,
or SEND is first identified, families need to know the great majority of
children and young people with SEND, with the right support, can find
work, be supported to live independently, and participate in their
community. Health workers, social workers, early years’ providers and
schools should encourage these ambitions right from the start”.
Autism Spectrum Disorder (ASD)
NICE guidance (2013) and (2017) regarding ASD in
under 19 year olds gives the following key recommendations:
- set up a local autism multi-agency group with managerial,
commissioner and clinical representation from child health and mental
health services, education, social care, parent and carer service users,
and the voluntary sector
- improve early recognition of autism by raising awareness of the
signs and symptoms through multi-agency training
- ensure relevant professionals are aware of the local autism pathway
and how to access diagnostic services
- consider a specific social-communication intervention for the core
features of autism in children and young people that includes play-based
strategies with parents, carers and teachers to increase joint
attention, engagement and reciprocal communication in the child or young
person.
Service Design and Delivery
NICE guidance (2018) covers services for children, young
people and adults with a learning disability and challenging behaviour,
recommending the adoption of a lifelong approach to supporting people,
their families and carers, focusing on prevention and early
intervention.
Social and Emotional Well-being: Early Years
NICE guidance on social and emotional well-being in early years
recommends adopting a life course perspective, recognising that
disadvantage before birth and in a child’s early years can have
life-long, negative effects on their health and well-being. Furthermore,
a focus should be put on the social and emotional well-being of
vulnerable children as the foundation for their healthy development, and
to offset the risks relating to disadvantage.
Social and Communication Skills
A research report conducted by Coventry University mentions SKILLS:
targeting social skills including greetings and goodbyes, nonverbal
communication, humour, conversation, perspective taking, emotions, and
friendship tips. An evaluation of the intervention reported an increase
in peer engagement and decreased isolation during playtime following
sixteen 30–45-minute sessions held twice weekly.
Further reported is The Conversation Club curriculum which focuses on
teaching participants basic skills identified as necessary for
successfully engaging in a conversation. These include:
- thinking about a conversational partner and remembering what they
have said
- selecting topics of mutual interest
- maintaining on-topic conversation by asking follow-up questions and
making comments
- demonstrating active listening
- using attention-gaining strategies to ensure partner is
listening
- repairing simple conversational breakdowns.
The Conversation Club curriculum is a nine-month programme where 14
lessons are repeated over a two-to-four-week period until participants
acquire the target skill. Research evaluating the effectiveness of the
Conversation Club curriculum reported increases in peer-directed
interactions, the number of questions asked, use of strategies to
introduce new topics, extended conversations on existing topics, and
attempts at conversational repair. Some evidence for increased use of
attention-gaining behaviours was also reported.
Engagement with Parents and Partners
Islington Clinical Commissioning Group in partnership
with the LA, have recruited and trained six local parents of children
with SEND to enable them to undertake parent to parent consultation to
inform local commissioning arrangements.
Consultations carried out so far have been to:
- support a local review of autistic spectrum condition diagnostic
pathways
- gain parents’ views of local effectiveness in identifying and
meeting the needs of children and young people with SEND.
East Riding of Yorkshire commissioned an external company to
undertake an independent strategic review of the continuum of support,
services and provision for children and young people aged 0–25 years
with SEND. This included engaging and gathering feedback from a range of
stakeholders, including young people, parents, carers and professionals
across education, health and care services. The overall aim was to
better understand how effectively the current range of SEND provision
was meeting the needs of children and young people, the identification
of gaps, and recommendations regarding how needs can continue to be met
going forward.
Strength-Based Practice
A strength-based (or asset-based) approach focuses on individuals’
strengths including their personal and social assets and their community
networks. It places the individual as well as their problems at the
centre of the process, highlighting ‘what is strong, rather than what is
wrong’. It helps to identify the resources within themselves, as well as
the support they have around them. It ensures the individual’s strengths
and talents are identified and considered in all interventions including
what is important for them or what they would like to achieve. Adopting
this approach from an early stage can be effective for children and
young people with SEND as it gives them a positive outlook for their
future.
Working with individuals through a strength-based approach is said to
improve individual outcomes, such as quality of life, employment, and
health. It promotes positive views of individuals and takes the focus
away from blame or judgement. This may contribute to de-stigmatisation
of certain groups including those with SEND.
Male Targeted Intervention
Future Men is a charity supporting boys and men, advocating for them
through informing policy and practice and delivering targeted programmes
and outreach work. Their work addresses some of the biggest societal
issues such as low educational attainment, poor mental health, and youth
violence. Males make up a large proportion of those children and young
people with SEND in Wandsworth (and indeed nationally), so male targeted
intervention and outreach work could prove effective. Disproportionate
identification of SEND within Black ethnic groups, particularly Black
Caribbean, is one of the most significant and long-standing issues in
Wandsworth and nationally.
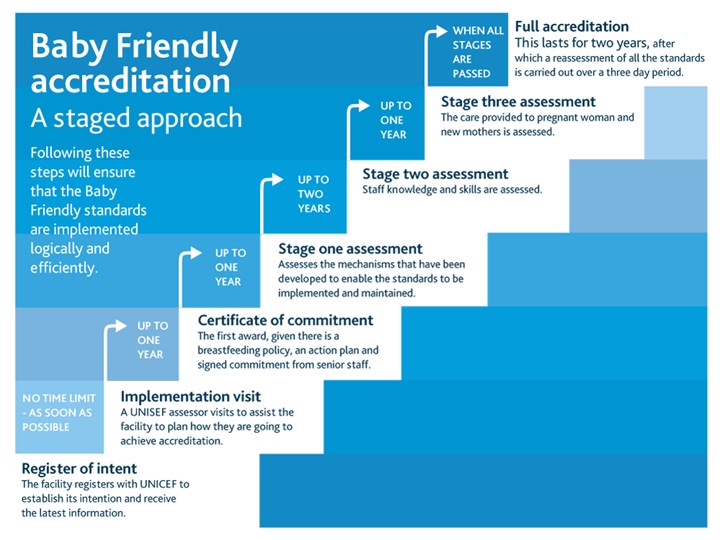
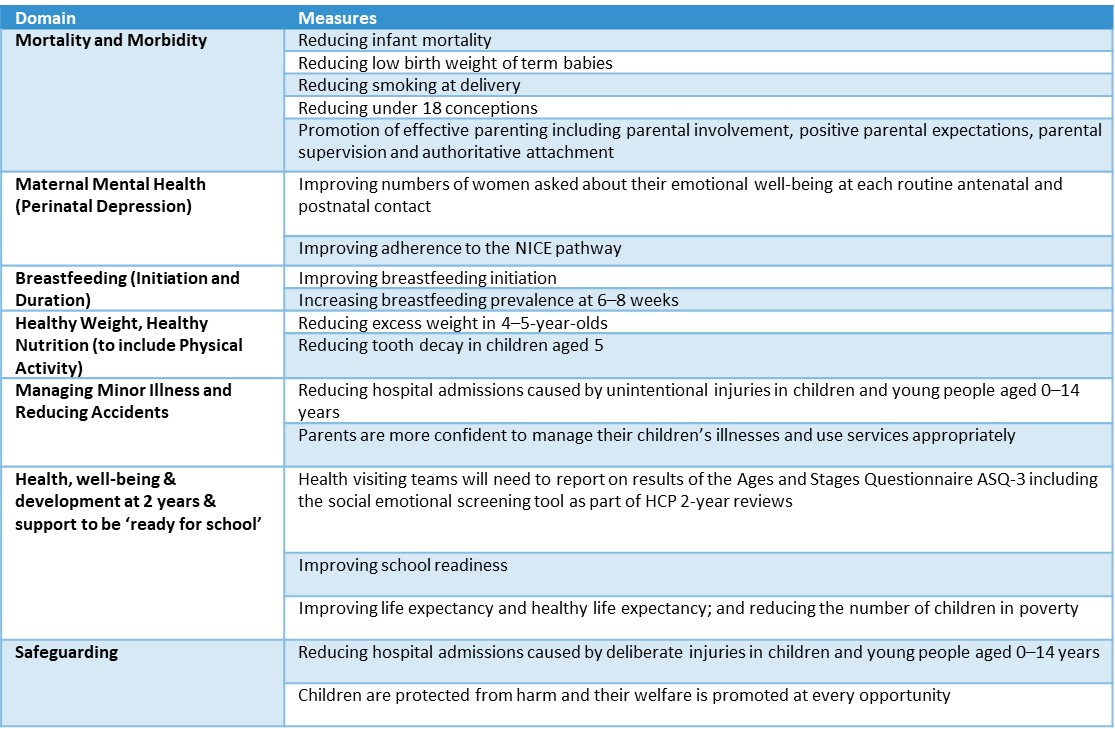
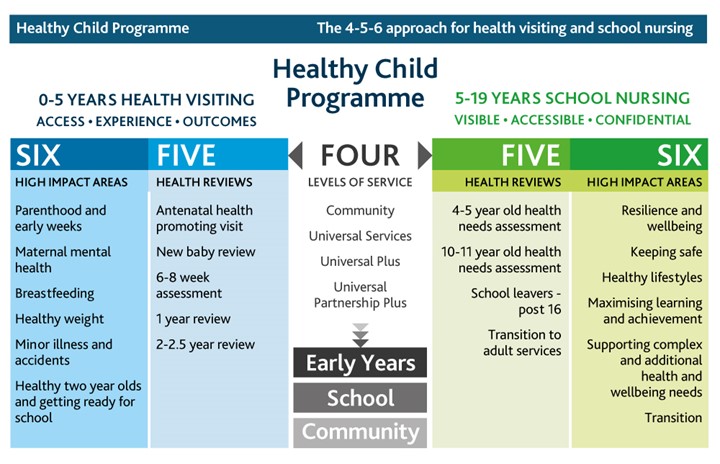
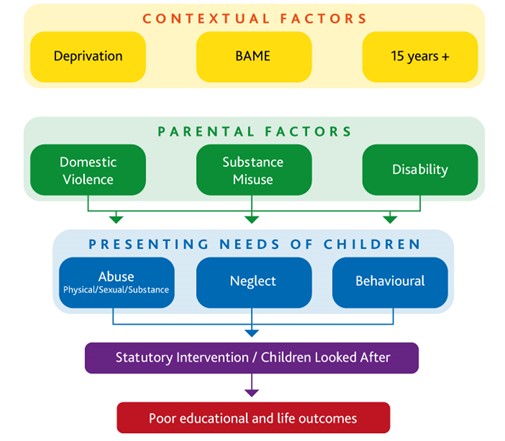
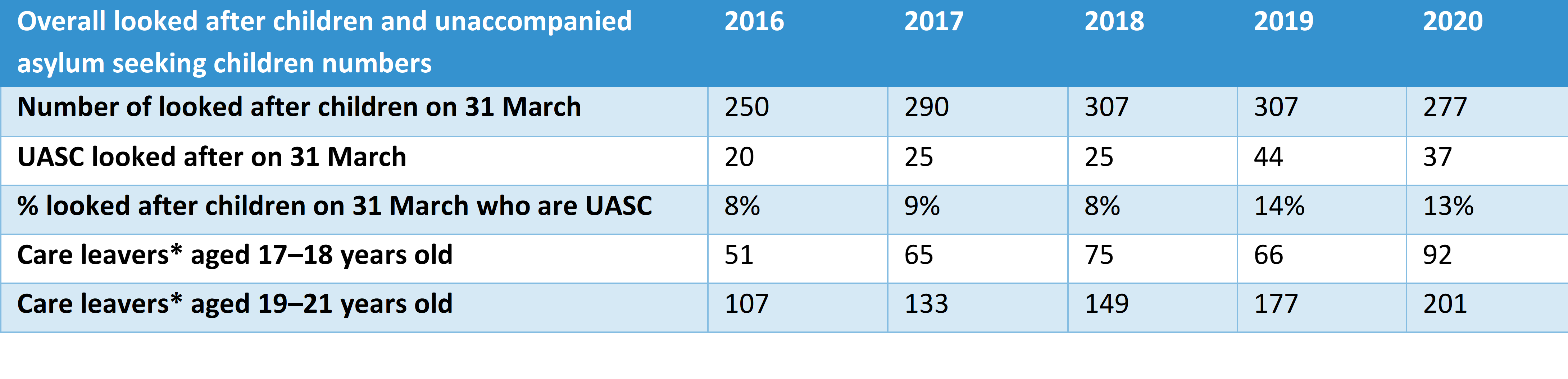
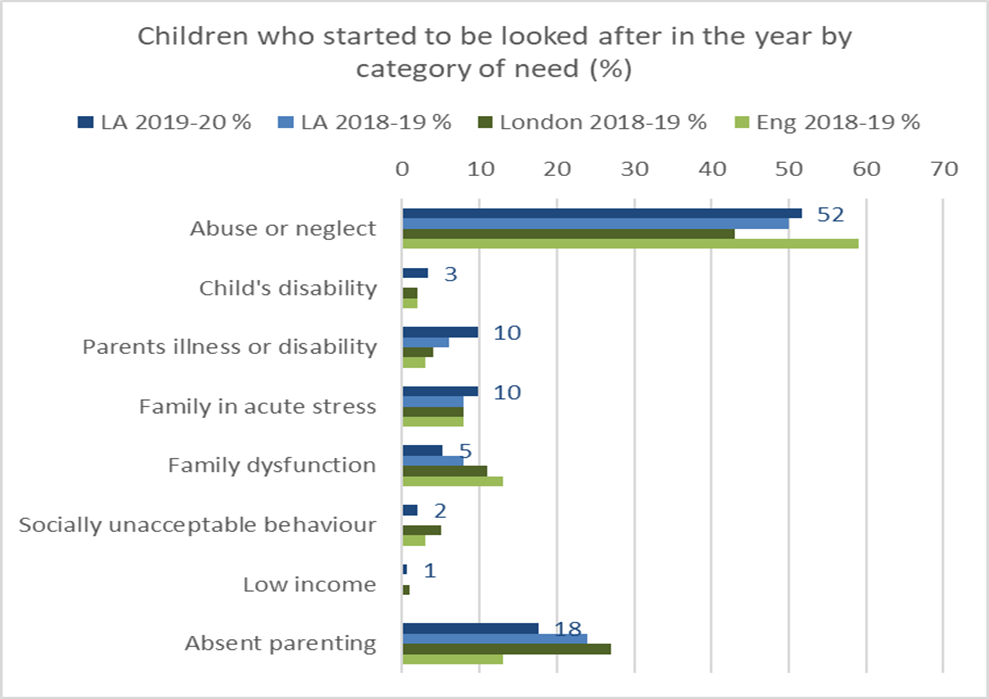
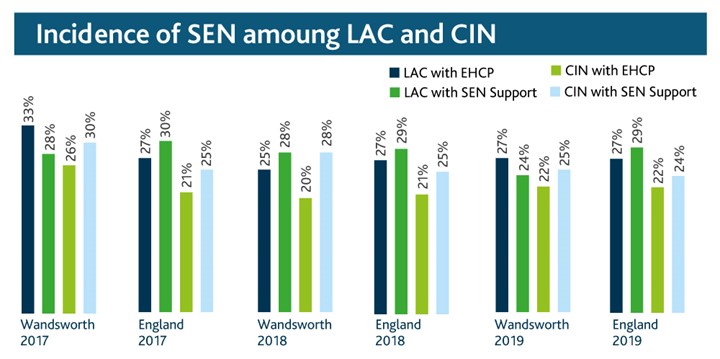
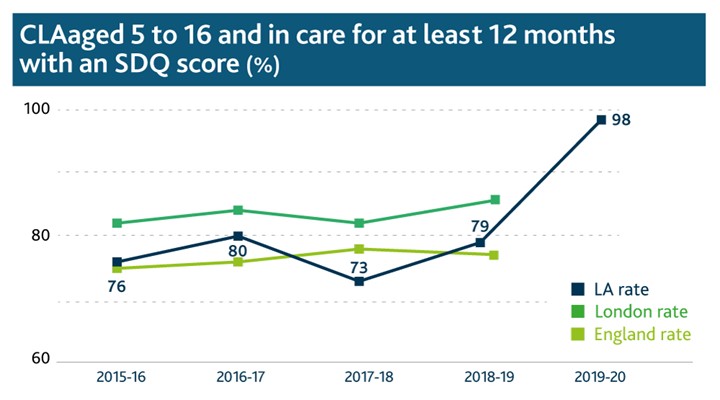
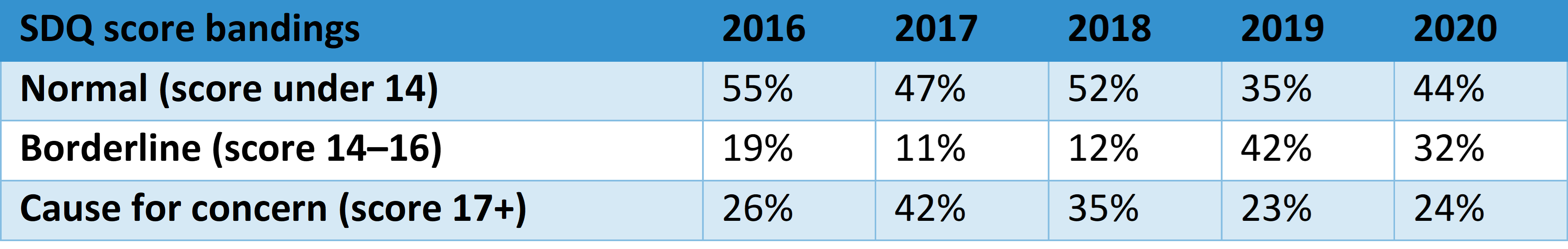
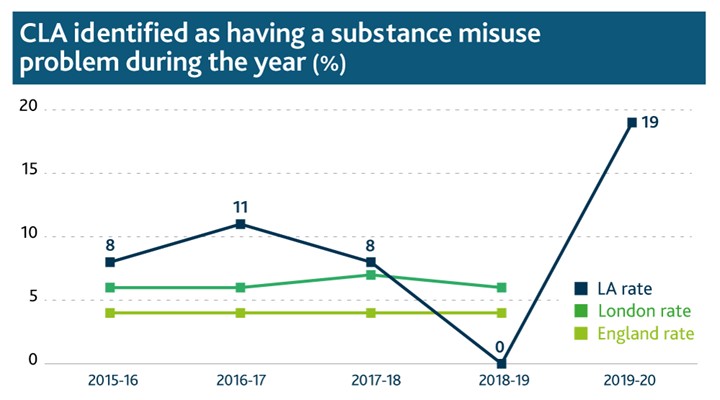
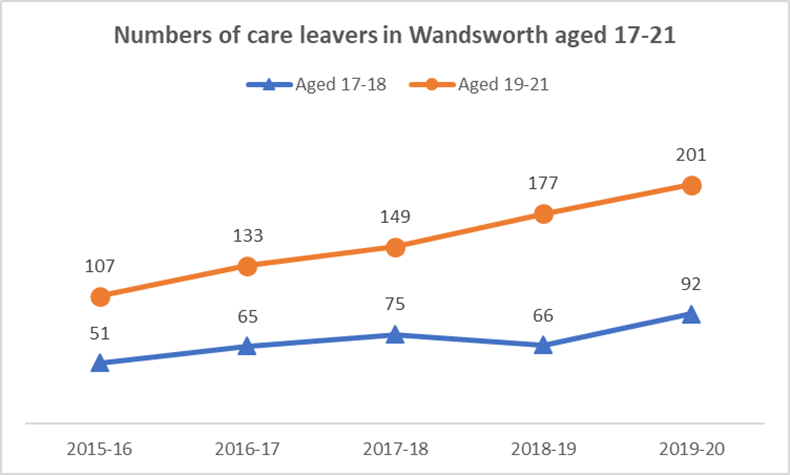
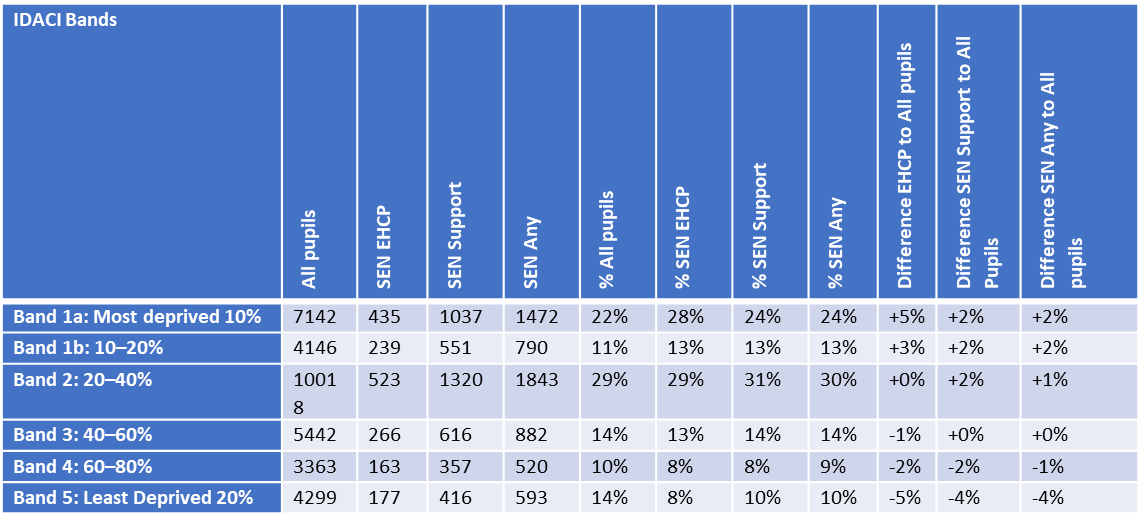
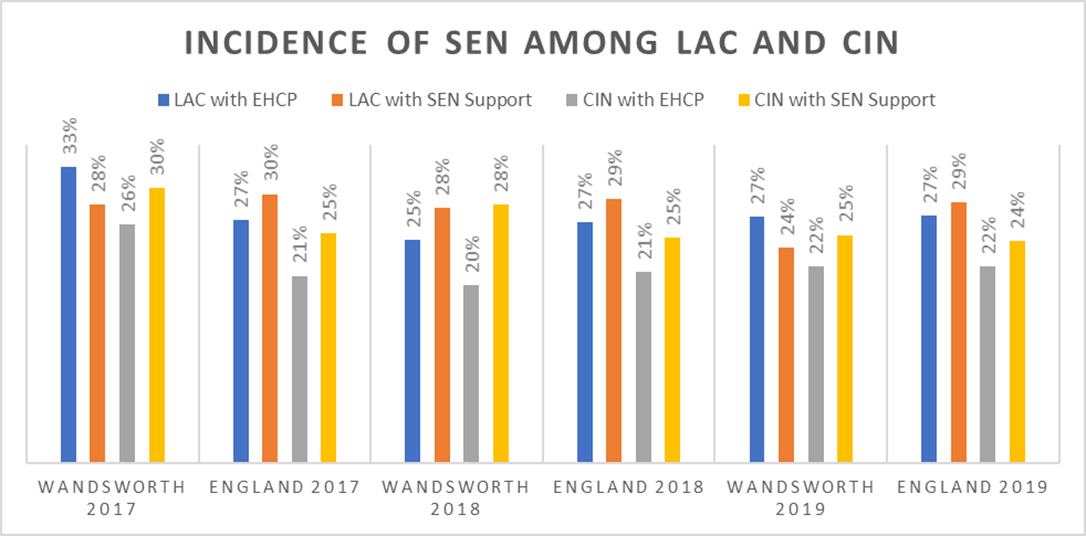
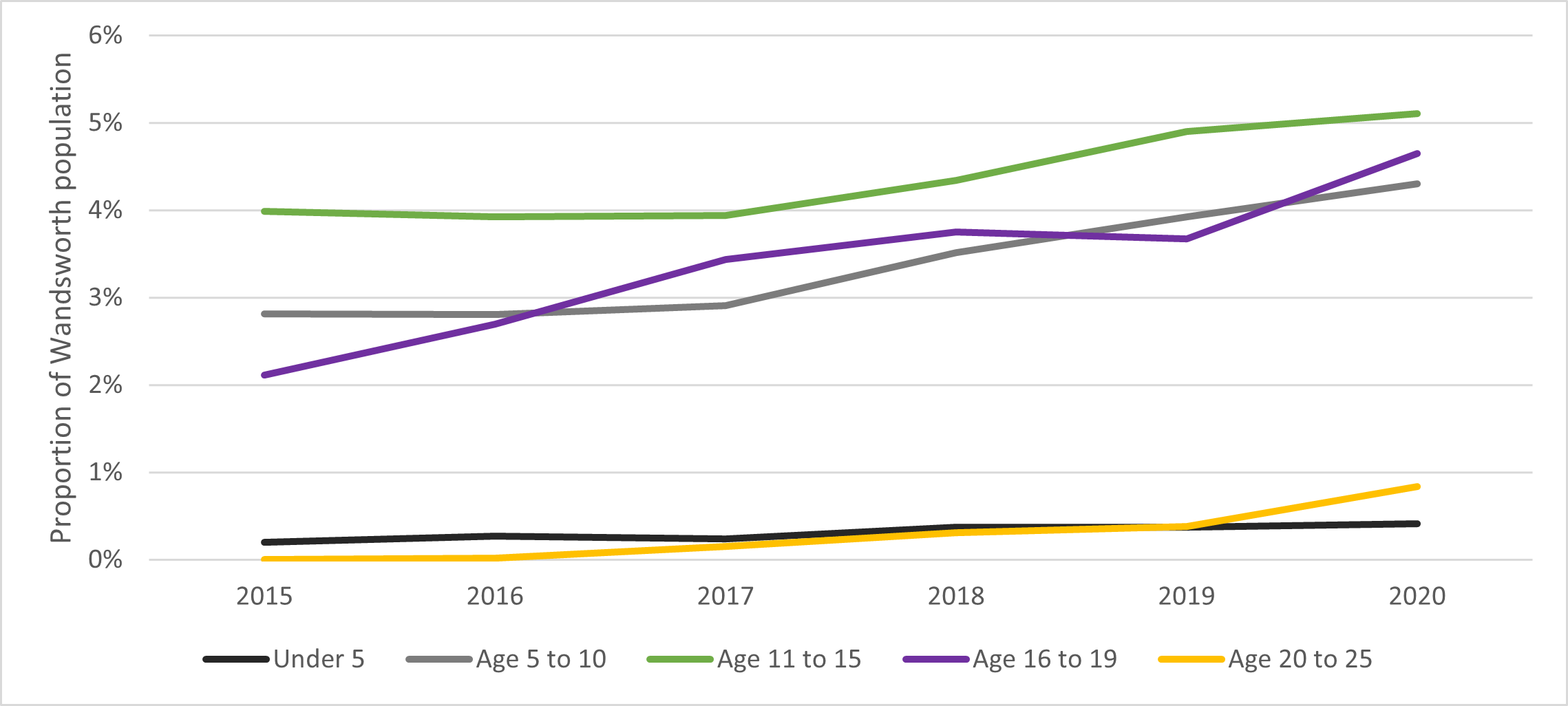
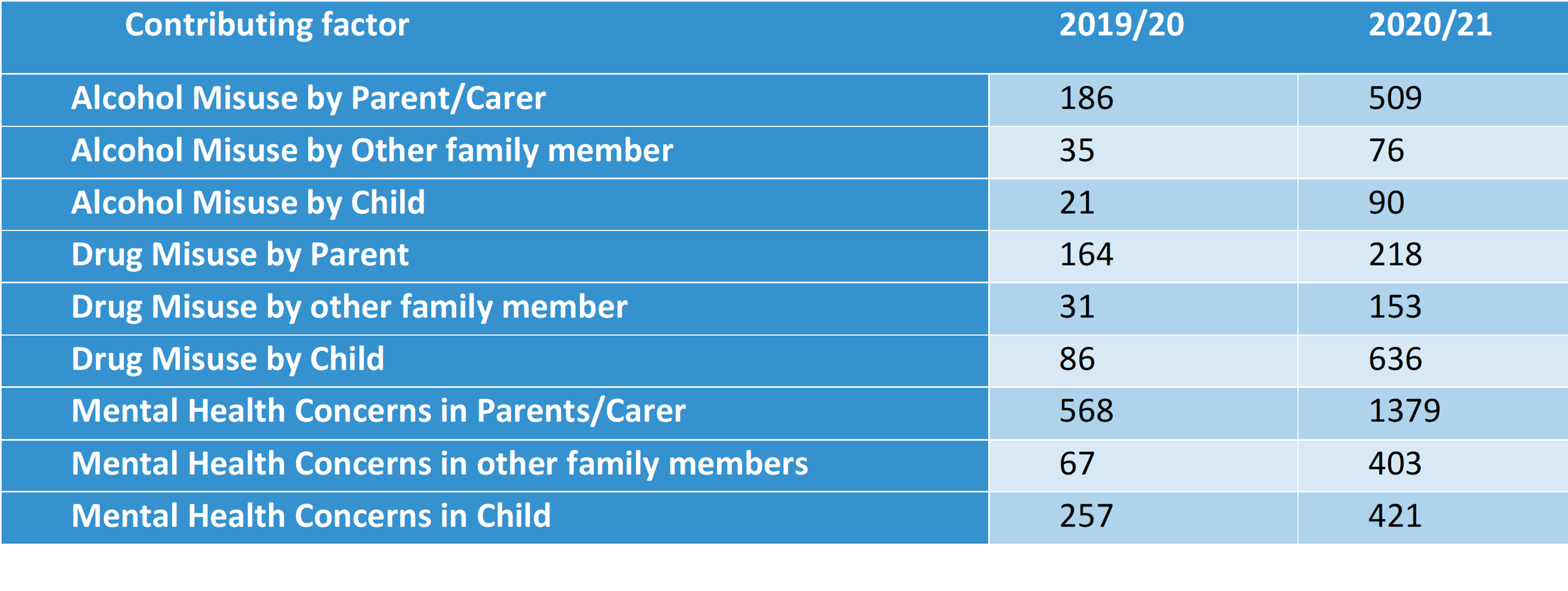

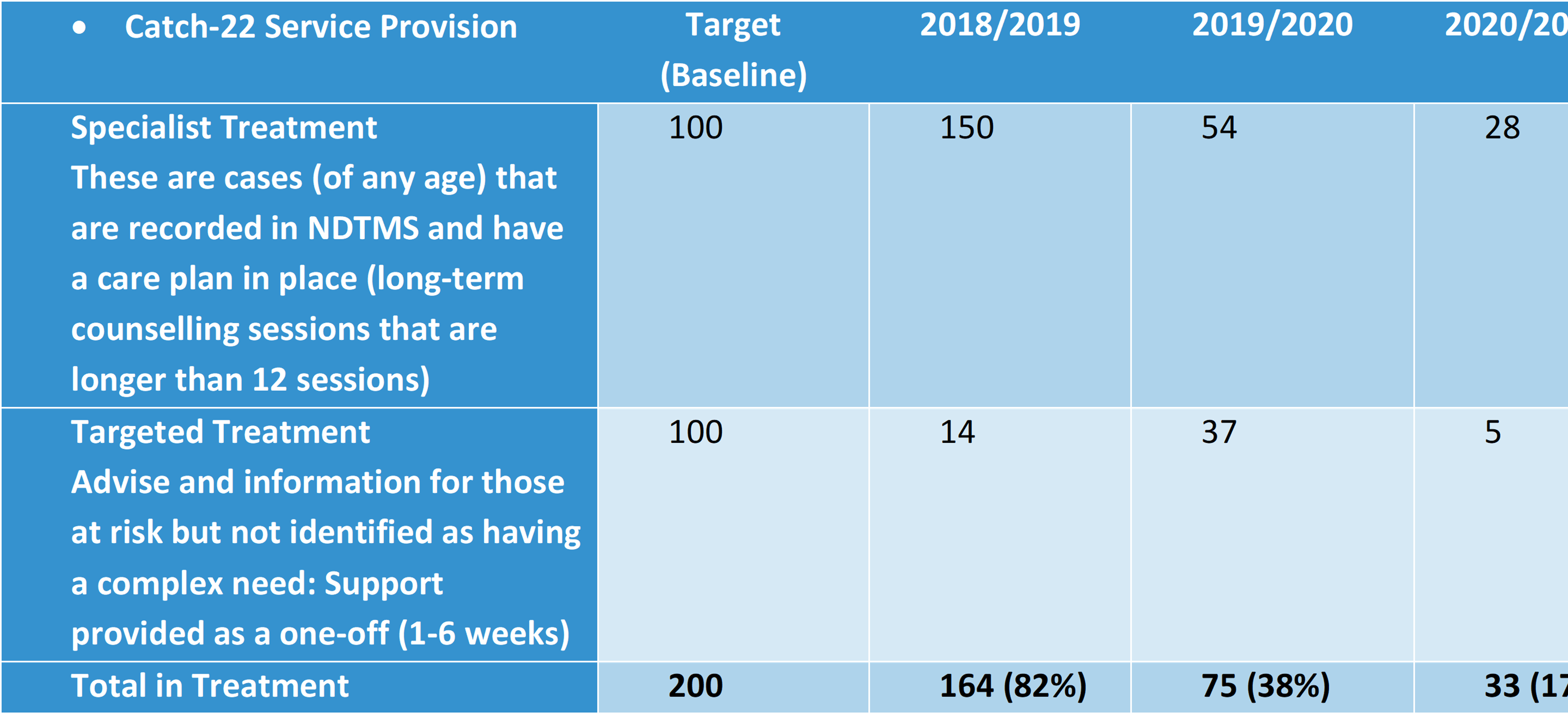
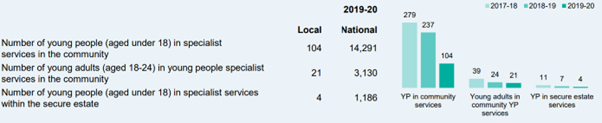
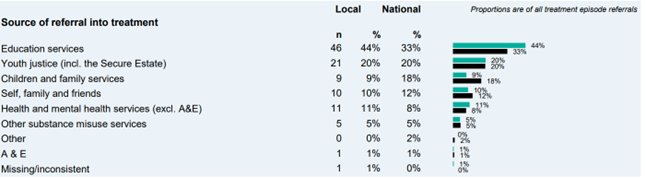
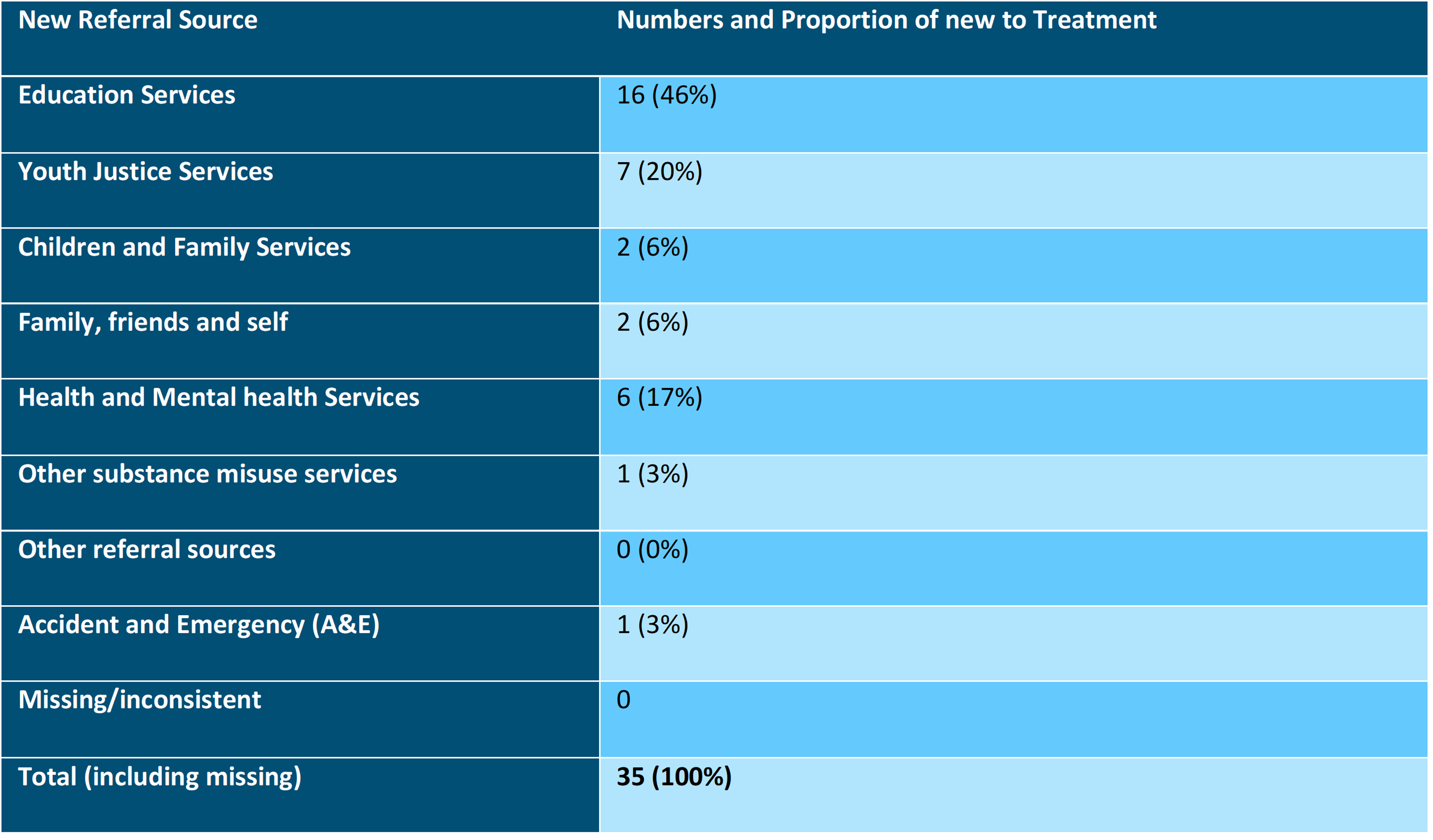
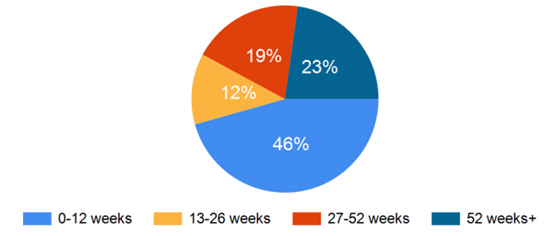
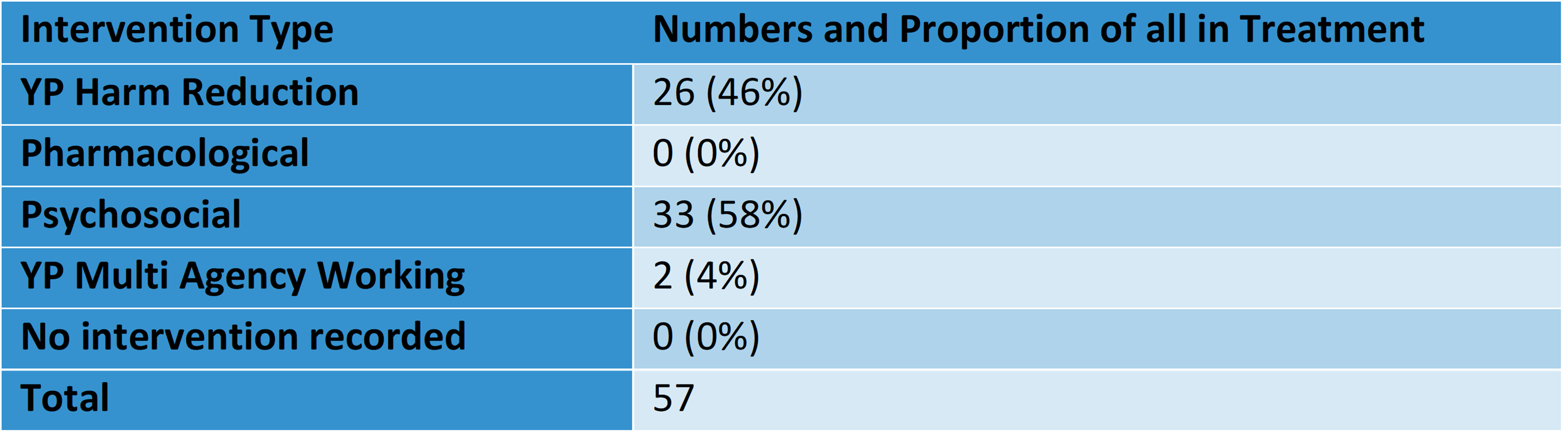
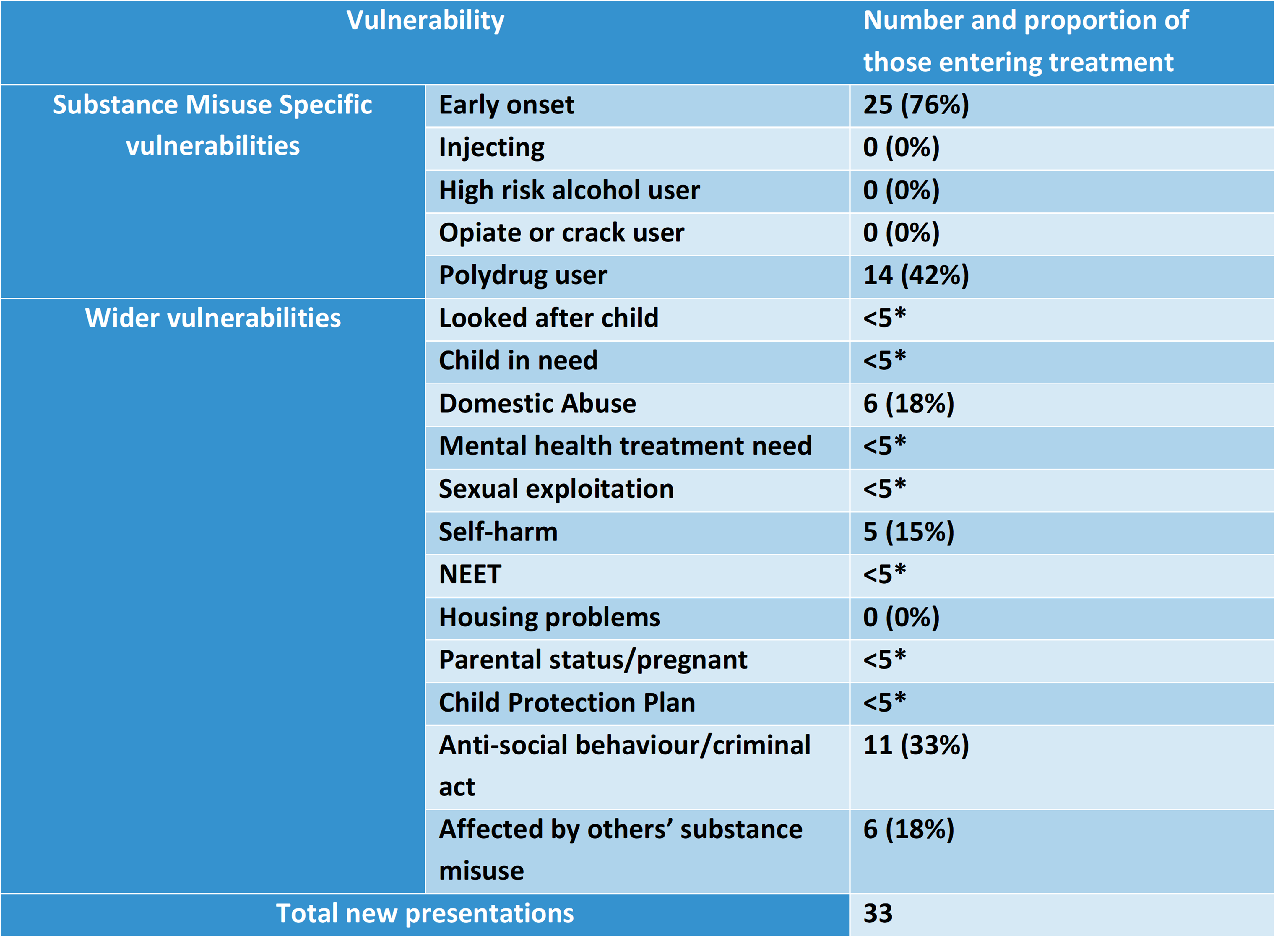
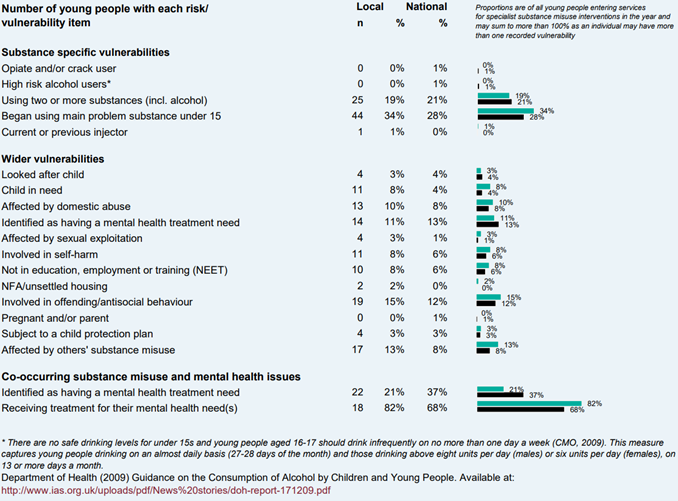
Social Work Practices
NICE guidance recommends publishing and regularly updating a directory of resources for looked after children and young people to aid social workers, and as a resource guide for looked after children, young people and care leavers 65.